A lecture I once gave at a nursing conference about workplace violence, hosted by the Marquette University College of Nursing, was followed by a vigorous question and answer session. After fielding a few questions, I noticed a woman in the front row sheepishly raising her hand. Frankly, she looked shell-shocked.
Her expression was blank and her eyes were wet with tears on the edge of spilling over. No one would even have noticed if I just ignored her and closed for the day, but something told me she needed to be heard and that we all needed to hear what she had to say.
I looked at her and nodded, saying, “Yes, in the front row?”
After a few awkward moments and in a trembling voice, she said, “But what about me? What about nurses?”
“Please, go on,” I said.
“What about all of us in nursing who have to deal with the disrespect day in and day out?” You could have heard a pin drop in that large lecture hall when a dozen side conversations just ended abruptly.
“Can you tell us what it’s like? The disrespect you experience at work?” I asked.
“I’ve been a nurse for 14 years, in critical care mostly,” she replied. “I work 12-hour shifts. I give my patients all that I have, emotionally and physically, and at the end of the day, I am exhausted. I get screamed at, threatened, or worse, almost every day I work. I’m not sure that I can go on doing this anymore.”
When I asked the group if anyone else felt that way, I was greeted by a lot of raised hands, nods, and knowing looks.
A new study reveals, yet again, that nurses are hurting from all the stress they experience at work. Stress from work-related trauma, long hours, and excessive conflict. And as the stress mounts with no end in sight, nurses continue to leave their proud and noble profession early, putting a larger workload on those remaining, which leads to more stress, more conflict, and so the cycle continues. Perhaps the most distressing part is that this study was completed just before the COVID-19 pandemic!
Conflict, Stress are common for all nurses regardless of specialty
The problem isn’t solely with critical-care nursing, the group addressed in this most recent study. Similar studies and surveys have found high levels of conflict and burnout among emergency nurses, home health nurses, sub-acute care nurses, and others. Higher levels of stress, turnover, violence-related injuries, poor job satisfaction, staffing shortages, poor worker physical and mental health, and increased medical errors.
So, the cycle of stress and conflict was there before the pandemic and it will still be there after the emergency has passed, but with even more nurses and other healthcare workers exhausted and leaving the front lines. The task ahead for post-COVID-19 recovery will be daunting just to return to the status quo. And the status quo was already unacceptable.
Do I paint a bleak picture? It might be an overstatement if the problem had not persisted throughout the entirety of my career, in healthcare. The old approaches of “killing them with kindness” and nurses telling themselves and each other that violence and overwork are just part of the job have failed them and their patients.
Nurses deserve better and so do their patients, because if we didn’t start taking better care of nurses, then we can’t expect better care for patients. Nurses and other direct patient care workers are hurting. And because they are hurting, healthcare is hurting. And because healthcare is hurting, patients are hurting.
The Ohio State College of Nursing Study, led by Bernadette Mazurek Melnyk, Ph.D., published in May of 2021 revealed the following:
- A large number of critical care nurses are in poor health and the statistics are alarming. Among a large study group, 3 of 5 nurses reported being in poor physical health, 1 of 2 screened for symptoms of anxiety, and 2 of 5 were positive for symptoms of depression.
- Critical care nurses who are in poor physical and/or mental health are 31% to 62% more likely to make medical errors, than healthy nurses.
Just as significant, the study indicated that when nurses perceive that their leadership is trying to support their wellness, nurses are twice as likely to be in good health, than those who didn’t perceive their leadership was trying to help.
[Critical Care Nurses’ Physical and Mental Health, Worksite Wellness Support, and Medical Errors, P.I. Bernadette Mazurek Melnyk, Ph.D., APRN-CNP Am J Crit Care (2021) 30 (3): 176–184. ]
But during my long healthcare career, spanning over 35 years, there had always been lavish support for employee wellness, no matter where I worked. Perhaps I was lucky. When I look back over my career, the steady stream of wellness initiatives seems endless.
The first hospital I worked at way back in 1991 provided a free 24-hour private workout center, complete with lockers and showers. They also had a sick child daycare center complete with on-staff nurses and local school district teachers, where employees could bring their sick kids who had to stay home from school, while they worked!
The second healthcare system I joined, in 1999, had wellness initiatives that involved free health screenings and extensive wellness-based programming. Participation even meant financial rewards, like significantly reduced monthly health insurance premiums.
We had ongoing health and wellness programming that all staff participated in at least monthly. Programming offered conditioning and weight loss programming that included reduced health club memberships, free nutrition coaching, sponsored athletic events, walkathons, free pedometers, competitions, free prizes, healthy food choices in the cafeteria, and on and on.
We had mandatory post-incident stress debriefings, access to free mental health counseling services, employee assistance programs, free marriage counseling, and even stress reduction massages scheduled on-site for free during work hours! But the turnover kept climbing and employee satisfaction scores kept falling.
The third and final healthcare system I joined had the same incentives and the same problems with morale, turnover, and employee health. So during my long career, I saw the same problems, the same attempted solutions, and very little progress.
Work-Related Stress & Work-Related Trauma
Nurses work long hours, of course, due to a long-standing nursing shortage that is worsening. Early indicators are even revealing that difficulty with anxiety and depression begins in nursing school. Difficulties with mental health and poor job satisfaction are situational and turnover, including job-hopping, are directly related to burnout, toxic workplace cultures, and workplace violence.
Perhaps the old adage, “nurses eat their young” reveals something endemic in the practice of medicine. Many doctors have a reputation for being kind to patients and mean, many even cruel, towards staff. Studies have shown a high prevalence of lateral violence, including bullying and even threatening behavior among medical staff of all levels to be problematic. It should be no surprise, in a profession that experiences some of the highest levels of disrespect and violence from its patrons. [Study: Prevalence of Horizontal Violence Among Emergency Attending Physicians, Residents, and Physician Assistants Nico B. Volz, BS,* Ryan Fringer, MD,† Bradford Walters, MD,† and Terry Kowalenko, MD† ]
Domestic violence and its aftermath are handed down often to subsequent generations when it is prevalent in the home; including, intimate partner violence, child neglect, and child physical and sexual abuse. Studies of trauma related to conflict and violence during early childhood reveal lifelong harmful impacts negatively affecting interpersonal relationships, professional success, physical and psychological health, and even life spans.
So perhaps it goes beyond the workload and into the experience and effects of work-related trauma. After all, many healthcare workers regularly see and do things that most people would consider life-changing events. So should we really be surprised that healthcare workers are unhealthy physically and mentally? In summary, the problems that healthcare providers have traditionally faced and continue to face are:
-
High levels of workplace conflict and violence: disrespect and violence from consumers is far more
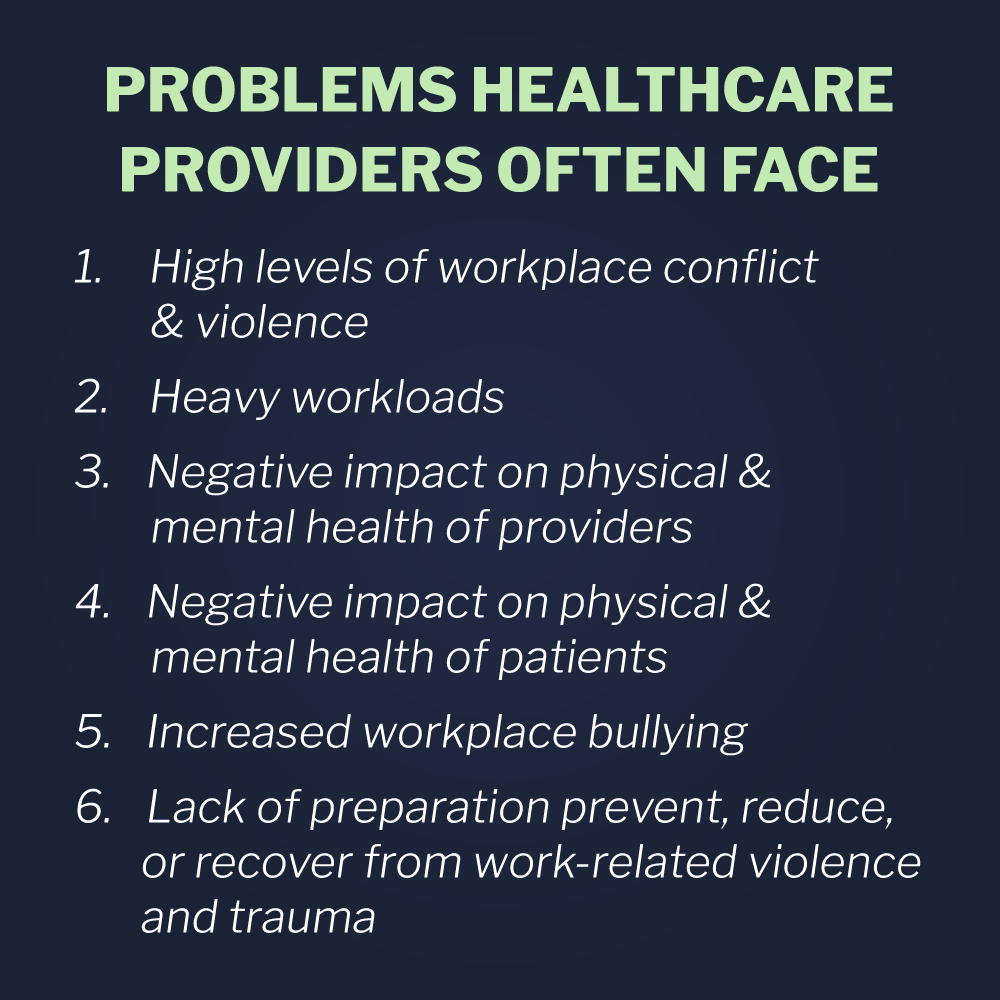 prevalent in healthcare than in other professions
prevalent in healthcare than in other professions -
Heavy Workload: healthcare staff, especially nurses, are leaving the profession due to job-related stress, creating increased workloads for peers and causing more stress and conflict
-
Harmful Effects to Providers: high levels of stress, conflict, trauma, and violence negatively impact the physical and mental health of nurses and other healthcare staff
-
Harmful Effects on Patients: the poor state of health among providers is leading to high levels of medical errors, leading to poorer patient outcomes
-
High Levels of Workplace Bullying: high levels of interprofessional disrespect and violence is endemic in healthcare
-
Traditional Approaches are Ineffective: healthcare staff are not sufficiently and properly equipped and prepared to prevent, reduce, or recover from work-related violence and trauma
The Ohio State study indicated that real solutions have immediate positive effects. Over half of the contributors to the Ohio State study reported better physical and mental health when they perceived their employers are taking concrete action regarding their well-being.
In healthcare, violence seems to have found a home. But is it possible to create environments of care that are incompatible with conflict and violence? Yes, it is. Vistelar’s training was developed by frontline professionals to address the full spectrum of conflict and violence, as defined and through the POLE acronym.
-
Physical: improved threat assessment and violence prevention
-
Organizational: improved job performance, morale, and collaboration
-
Legal: protection from personal liability, career pitfalls, and damaged reputation
-
Emotional: improved relationships, self-confidence, and quality of life
Vistelar's Conflict Management Training Can Help
At Vistelar, it begins with our core principle of treating people right, by showing them respect. We not only ask people to treat others with respect, but we train them how to do it, through job-related, scenario-based, professional communication training. Participants in training actually practice the Five Approaches for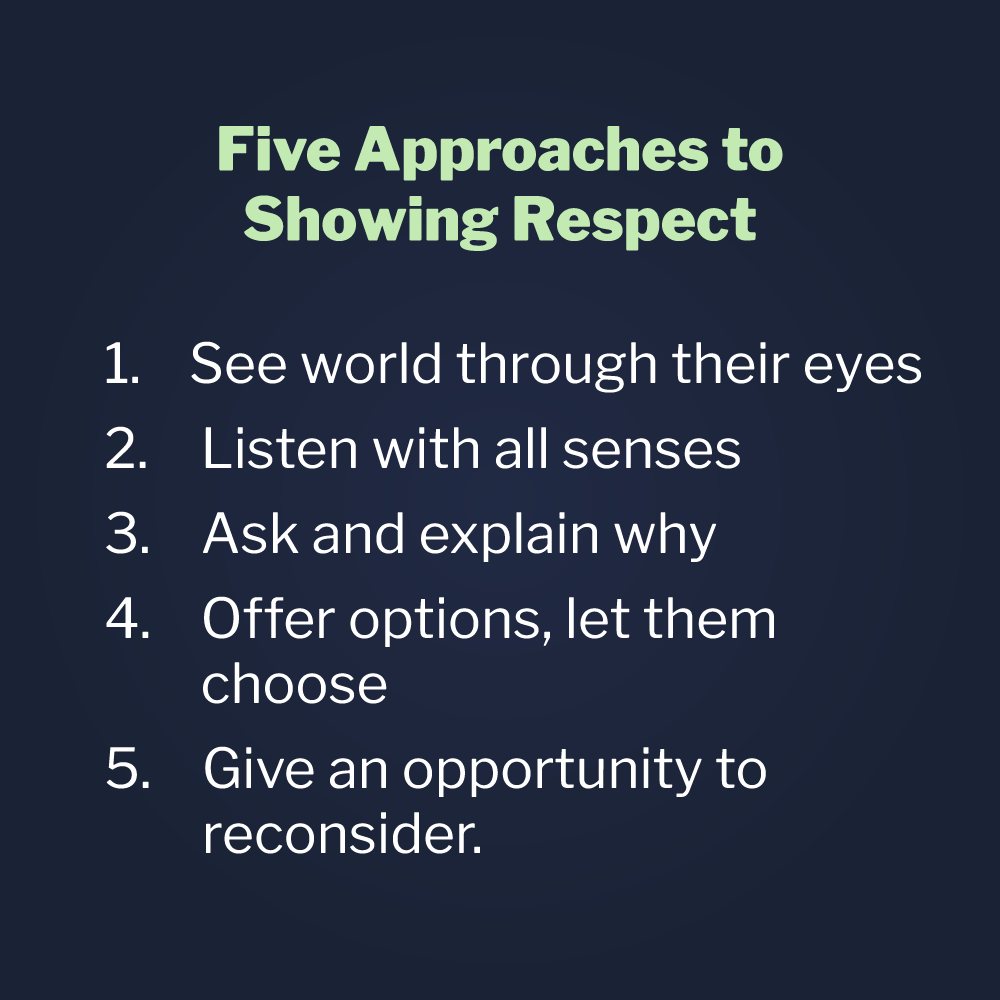 Showing Respect, which are: 1. See the world through their eyes, 2. listen with all your senses, 3. ask and explain why, 4. offer options, let them choose, and finally, 5. give an opportunity to reconsider.
Showing Respect, which are: 1. See the world through their eyes, 2. listen with all your senses, 3. ask and explain why, 4. offer options, let them choose, and finally, 5. give an opportunity to reconsider.
And the five approaches are just the beginning. Vistelar’s programming involves scenario-based training for non-escalation, how to prevent conflict; de-escalation, how to reduce conflict, and crisis management by learning what to say and do to keep people safe when others have lost their ability to cope.
Beyond that, even though they will already be far more successful at preventing and reducing conflict, crisis, and even violence, participants in Vistelar’s programming are empowered with Personal Protection and Positive Interventions and Stabilization training, for those times when healthcare providers must take action to protect themselves and their patients, all while looking professional, demonstrating concern, and keeping everyone as safe as possible.
From beginning to end, Vistelar addresses the entire spectrum of conflict and violence, culminating in the principle of Closure, where healthcare professionals learn to keep themselves and others safer, even when the outcomes are not what patients, families, and providers would have preferred.
Click here to read An Evaluation of of the Vistelar Training Initiative at Milwaukee County Behavioral Health Division: Final Survey Report.