Enjoy this excerpt from one of our published books.
Chapter 5
The Cold Supper Tray:
Beyond Active Listening
“There is, however, a limit at which forbearance ceases to be a virtue."
-Edmund Burke
One evening, while supervising security in a hospital, I was sent to a nursing unit subsequent to an assault on a nurse. The security team arrived ahead of me and the situation had already quieted down. The officers and I debriefed the incident among ourselves, before they returned to regular duties. They reported to me that the floor was already quiet when they arrived so I stayed behind to tie up the loose ends. No injuries were reported and all appeared well; however, when I debriefed the nursing staff a different story started to unfold.
The nursing supervisor complained that this particular mother of a patient was verbally abusive and sometimes even threatening towards nursing staff. I asked how long this had been going on and she said about a week. When I asked if she’d reported anything to security before tonight she said she hadn’t nor had anyone else. When I looked through the medical record there were no social work or nursing notations about the mother’s supposed weeklong abusive behavior. It was unfortunate that the unit staff had waited so long to ask for help. In all likelihood, this incident could have been avoided if we had been able to rein in this mother’s behavior when it first started. Addressing her behavior at this late stage was going to be much more difficult.
The incident went something like this: the patient’s evening meal had been delivered, along with a visitor’s meal for the mother. The mother was displeased with the meal and threw her tray at the patient’s nurse. The tray missed her, but smashed against the wall causing the nurse to run from the room. After hearing this, I decided to speak to the mother.
“Don’t go in there!” said the nursing supervisor. “You’ll just make things worse.”
“Her behavior was pretty outrageous,” I replied. “You also said she’s been going on like this for a while. Don’t you think we need to get to the bottom of things and set some limits on her behavior?” I asked.
“Not right now. We just got her calmed down!” she pleaded.
“I understand how you feel, but I have to make an assessment and set some limits,” I replied. “I’ll try not to make things any worse.”
When I arrived at the room the door was half open. It was dark inside and quiet, except for the low volume of the television set. I knocked on the doorframe and the mother said, “What do you want?” in a stern tone of voice. With that I opened the door all the way and stood just inside the doorframe, where I could see the room and assess for any hidden dangers. I could also exit the situation quickly if she decided to start throwing things again! When I saw the scene was safe, I started in with my Universal Greeting.
“Hello, Ma’am. My name is Joel. I’m the security supervisor on duty.” She just stared at me blankly, so I continued. “The reason I’m here is because of the incident that just happened. I need to get your side of things. Can you tell me what has you upset tonight?”
“I’m not upset, everything is fine, I don’t need to talk to you,” she said, matter-of-factly.
“I understand what you’re saying ma’am, but I have to talk to you about the incident. Can you please tell me what happened?” While talking, I had entered the room and closed the space between us to about five feet.
Then she looked up at me and continued, “These nurses are disrespectful. They’re rude and act like they’re better than me. And they aren’t taking care of my child properly!”
Showing Empathy
“Well, I understand now why you’re angry. Have you complained to the charge nurse or a supervisor?“ Before she could answer, I blurted, “How’s your daughter doing, by the way?” This is an important point in the conversation for healthcare workers. Again, in healthcare we have a built in emotional or practical appeal. Drawing a patient’s attention to their own condition, or even a visitor’s or family member’s attention to their loved one’s condition, can go a long way to showing Empathy and resetting their state of mind.
she could answer, I blurted, “How’s your daughter doing, by the way?” This is an important point in the conversation for healthcare workers. Again, in healthcare we have a built in emotional or practical appeal. Drawing a patient’s attention to their own condition, or even a visitor’s or family member’s attention to their loved one’s condition, can go a long way to showing Empathy and resetting their state of mind.
“She’s doing better,” replied the mother.
“Great, is she going home soon?” I asked.
"We were supposed to go home tomorrow,” she answered in a trembling voice.
“Well, I hope she is well enough to go home soon, if not tomorrow.” I then continued with some probing questions to clarify the situation in my mind. “Can you tell me what happened tonight? The nurses said you threw a tray.”
“My food tray was cold! I’m tired of being treated like this!” she said tersely.
Let me see if I understand what you’re saying,” I asked. At this point, I was preparing to Paraphrase what she had just said. Paraphrasing is a powerful tool in conversation. It’s a way of getting people to focus, as everyone generally will give you their full attention whenever you say you are going to tell them your thoughts on what they’ve just said. You can even politely interrupt by saying something like “let me tell you what I think you mean.”
Paraphrasing also serves as a sort of mirror that reflects the other person’s behavior back at them. “So you’re saying that you threw your tray at the nurse, smashing glasses and plates on the wall and causing her to run from the room because your dinner was cold? I have to write a report so I really want to make sure I get your side of things.” At that point she hung her head and started to sob quietly, so I just continued. “Ma’am, I know something’s wrong and I want to help. I don’t think you threw your tray at that nurse just because your meal was cold. Can you tell me what’s really wrong so I can help you?”
“Yeah, well,” she said softly before continuing. “My no good husband gambled our rent money. My daughter is getting out tomorrow and we don’t have anywhere to go.”
That was my opening to Summarize the situation for her and move towards some resolution. “I’m glad you confided in me, Ma’am. Here’s what I can do. With your permission, I can ask the on-duty hospital social worker to stop up tonight. She may have some options to help in this situation. We don’t want to discharge your daughter to the street. Your doctor and the hospital administration will want to know what’s going on and will try to help if you let them. Also, if you want to see about counseling for your husband’s gambling, she will have resources for him.”
She sighed deeply before answering in a sheepish tone, “Yes, I would like to talk to someone.”
“I’m only too glad to help you and your daughter. However, you understand that if you had hit that nurse with that tray, you’d probably have been arrested for an assault. Then you would be in jail, your daughter would still be in here, and your rent would still be unpaid.”
“I’m sorry. I wasn’t trying to hit her,” she replied.
“I’m really glad you didn’t. If at any time you feel that you’re being treated unfairly, talk to the charge nurse or a supervisor. You could also ask to talk to someone from patient relations. Now that you know what to do if there are problems, I’m asking you to please stop yelling and cursing at your daughter’s nurses. I can’t help you unless you show them respect.” She nodded in agreement, so I continued, “There are also other kids on this floor and this has to be a safe, quiet, and appropriate environment for them as well as your daughter.”
Before leaving the unit, I debriefed the nursing staff. I shared with them her assurances that she would show them respect. I asked that they address cursing, yelling, and name calling immediately and that they should call security for support, before things got out of hand again. Perhaps, most importantly, I shared the mother’s perspective that she felt disrespected by some of the nurses. I also shared that she was struggling with some very profound family issues, causing her to be fearful about her daughter’s future after discharge.
The patient and her mother were on the unit for another three days without incident. I checked in often to see how things were going and the nurses related that the mother had “opened up” to many of them and was generally pleasant. The mother related to me that the nursing staff was much more supportive and approachable. On the final day the nursing supervisor asked me what many doctors, nurses, social workers, and hospital security people have asked me over the years, after dealing with difficult patients and families.
She asked, “What exactly did you say to her?”
Beyond Active Listening
In the final analysis, it isn’t as much as what we say with our words as what we “do” with them. As for the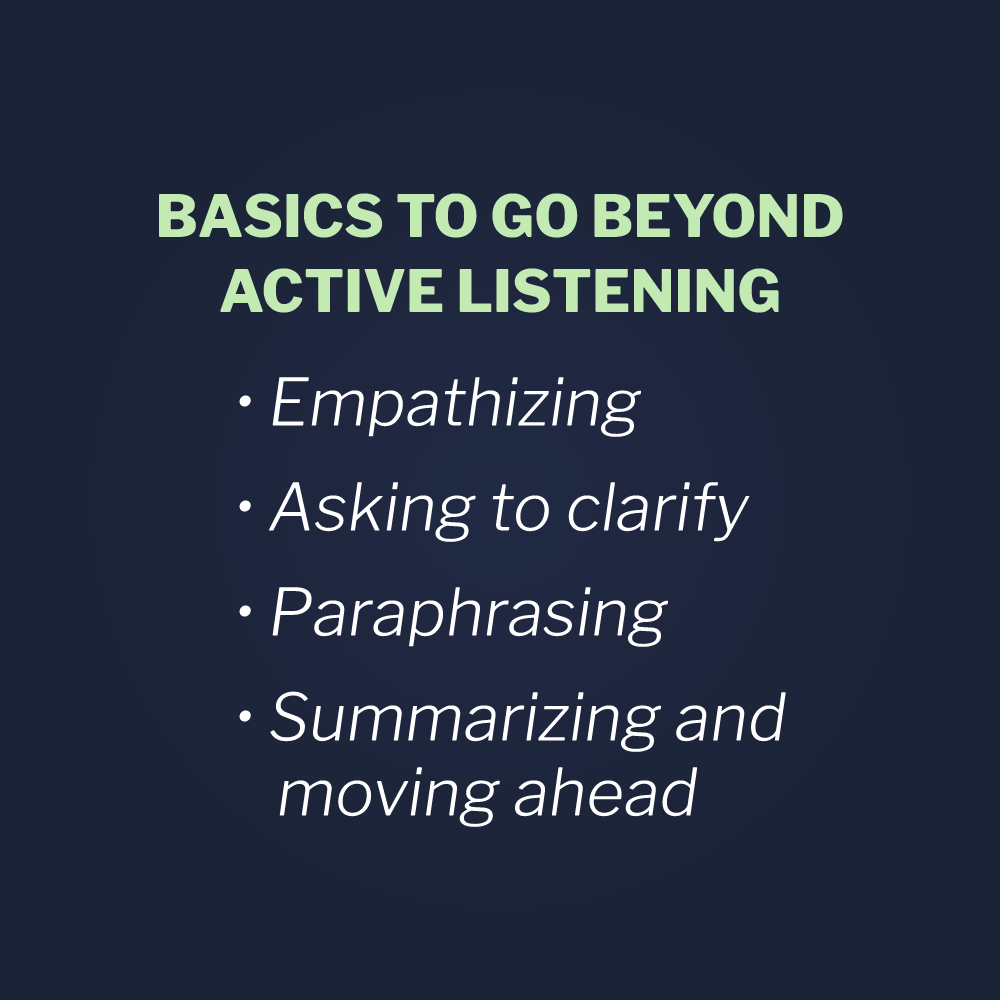 angry mother in the preceding story, I established communication with a Universal Greeting and empathized with her situation, while not entirely agreeing with her point of view. We can show Empathy with someone’s situation without legitimizing bad behavior, by simply acknowledging their illness, their situation, or even their anger. I also asked questions to Clarify her point of view, while mining for details. People aren’t usually forthcoming when being called-out on their behavior, so clarifying questions are essential for getting them to open up. Then, I shared my understanding of both the situation and her point of view by Paraphrasing. By doing so I was able to focus her attention and reflect her behavior back for her to examine objectively. Finally, I was able to Summarize—problem solve, set limits on future bad behaviors and offer appropriate solutions for future problems.
angry mother in the preceding story, I established communication with a Universal Greeting and empathized with her situation, while not entirely agreeing with her point of view. We can show Empathy with someone’s situation without legitimizing bad behavior, by simply acknowledging their illness, their situation, or even their anger. I also asked questions to Clarify her point of view, while mining for details. People aren’t usually forthcoming when being called-out on their behavior, so clarifying questions are essential for getting them to open up. Then, I shared my understanding of both the situation and her point of view by Paraphrasing. By doing so I was able to focus her attention and reflect her behavior back for her to examine objectively. Finally, I was able to Summarize—problem solve, set limits on future bad behaviors and offer appropriate solutions for future problems.
These techniques are part of the skill set of the Beyond Active Listening tactic that providers are trained to use in Vistelar’s conflict management training course. By building competence in this tactic and applying it early in the cycle of violence, situations like the one above can be avoided and clinical relationships can be strengthened even under the most trying circumstances. Going Beyond Active Listening isn’t just for setting limits on known behaviors, but also for getting to the root of both real and potential problems.
Every provider knows patients who had poor outcomes and were still grateful for the care they received. They also know patients who had stellar outcomes but still filed several complaints and treated staff disrespectfully despite every effort being made to ensure their satisfaction. A patient’s perception of the care they received is connected not only to the outcomes of therapy, but also to the environment in which that therapy was delivered. Was it quiet? Was it safe? Was it clean? Was the staff friendly and approachable? Any one of these lynch pins, if pulled out of place, can collapse the overall favorable perception of the quality of care.
Gateway Behaviors of Violence
This may be especially true, in relation to the Gateway Behaviors of Violence. If a patient’s life is on the line, their choice of hospital is primarily based on its resources and reputation, within the constraints of their financial resources and insurance policy. But for routine hospitalizations and urgent care needs, they will more likely choose comfort and safety over reputation and even location. This is a dynamic I’ve witnessed many times from both sides. I have worked in top-notch facilities that people refused to patronize because the perception was that they were unsafe. I’ve also worked in others that were out of the way and of average reputation that people drove long distances to get to because the perception was that they were safer than the ones in their own community. Sometimes that perception was connected to a hospital or clinics’ location in a high-crime area or just the fact that it was located in a major city. Often, however, it was connected to something they had seen or heard when they were once in the emergency room at that hospital or visiting one of its clinics. Sometimes, it was based solely on its reputation as an unsafe place.
The Universal Greeting combined with Beyond Active Listening form a skill set providers can use to set and maintain a Social Contract that promotes patient satisfaction. That said, the pendulum swings both ways. One of the things providers complain about a lot is the tension that some patients and even family members bring to the bedside. Often, that tension is something they can’t put their finger on. Sometimes it’s just a look, a sigh, or just a “feeling” that patients and visitors bring to a therapeutic relationship. “What’s the harm?” you might ask. The harm caused by undefined “tension” is that it directly impacts the perception of the care the patient is receiving.
Complaints are more likely generated based on a patient’s or family member’s attitude and have little or nothing to do with the actual quality of care that they received. The point being that patient satisfaction isn’t solely connected to the quality of care, but also to the beliefs and attitudes the patient brings to the environment of care. But what, if anything, can we do about that?
People can be categorized into three personality types for the purpose of training. The first are “yes” people. They are the ones who are positive in their dealings with everyone. “Yes” people are the ones who are generous and understanding even when things don’t always go well. However, if “Yes” people are handled improperly, even their goodwill can be eroded.
Then there are “No” people, who are hard to satisfy and overly suspicious. They are the ones who often refuse to cooperate, the first time they are asked to do something. However, in the hands of a skillful communicator, they can be persuaded to comply.
The last are “passive-aggressive” people. They appear to be “yes” people, but are actually “no” people.” Passive-aggressive people hide their real purpose, their real feelings, and their real attitudes. Their complaints come out of left field and they only make them if there is no personal risk involved. These can be the toughest people to manage. Passive-aggressive patients may appear satisfied and never complain to the provider face-to-face, but then throw them under the bus to other providers, administrators, other patients and visitors.
Passive-aggressive staff members can do serious damage to the environment of care. Passive-aggressive behavior is a category of conflict on which I am frequently asked for advice, whether it’s peer-to-peer or directed against providers from patients and families. Among peers, in the healthcare profession, it is commonly referred to as lateral violence or systemic bullying. According to the American Nurses Association, well over half of the nurses they surveyed in 2001 reported having been verbally abused or threatened by peers or people in authority.
A 2004 study from the Institute for Safe Medication Practices found that 48 percent of nurses, pharmacists and other healthcare professionals reported experiencing verbal abuse from peers and 43 percent reported intimidating and threatening body language. Perhaps most disturbing is that 40 percent of respondents reported “keeping quiet” when noticing medication errors due to an intimidating colleague, yet another way that violence affects patient health and safety.
The Impact of Lateral Violence
Lateral violence from peers, just like violence experienced from patients and families, also affects staff performance by its negative impact on overall morale and increasing absenteeism and turnover. This is a particular concern considering we are currently experiencing a national nursing shortage. Therefore, lateral violence, just like any other form of healthcare violence, is affecting the public health. Studies have also documented the negative effect of lateral violence on patient health and safety, while still others have revealed its impact on providers themselves. The effects of lateral violence in healthcare include higher levels of anxiety and anger that can lead to depression, hypertension, and even coronary heart disease.
Recommendations for dealing with lateral violence range from raising awareness to policies protecting whistle blowers and zero-tolerance for bullying. But how do we manage behaviors, such as gossiping, ostracism, excluding and the withholding of information? What about intimidating behavior, such as the looks, sighs, and “feeling” that can permeate an office or nursing unit? Beyond Active Listening is clearly one skill set we can teach clinicians and managers to protect their working environments and empower providers to protect themselves. Especially since nursing is thought to be one of the professions where lateral violence is most prevalent and its affects most devastating. Bullying is no secret among members of the healthcare profession and perhaps that’s why the expression, “Nurses eat their young” is so widely known.
What about those patients and family members who negatively impact the environment of care and ultimately affect their own outcomes? When patients and visitors are rolling their eyes, addressing us in an irritated tone of voice, or conspicuously ignoring us, we need to call those behaviors out into the sunlight. Skilled providers using the Beyond Active Listening technique can set and maintain a better, safer, and more therapeutic Social Contract with their patients.
“Hello, Mrs. Davis. I’m Julia, your mother’s nurse this evening,” she said smiling and in whispered tones, as her patient was sleeping. “I just stopped in to get her vitals. Can I get you anything afterwards?”
“No,” replied Mrs. Davis shortly, never looking up from her magazine to make eye contact.
“Her pulse is strong and her blood pressure is very stable tonight, that’s good,” whispered the pleasant nurse.
“Whatever you say,” said the visitor, while rolling her eyes, shaking her head and smirking disapprovingly.
“Ma’am, I know you’ve been here a long time and you seem worried. Can I help? Maybe I can answer some questions?”
“There’s nothing you can say to me,” said the visitor.
“Well I can see that you’re upset about something and I just want to help.”
“I’m not upset,” replied the visitor.
“Okay. I just want you to know that I’m here for you if you need anything or if you have any concerns. It’s no fun being cooped up all day and worrying about your mother. Can I get you some blankets, pillows, some coffee or something? Maybe I could check around and find some better magazines?” she offered while wearing a look somewhere between a smile and a look of concern.
The visitors grim face softened and she looked the nurse in the eye for the first time, saying, “I’m sorry I’m such a b***h.”
“Oh, not at all, Mrs. Davis,” replied the nurse.
“I don’t mean to take it out on you. You’re such a sweet girl. My mom is lucky you’re here for her. I’m just tired and worried, like you said. And these magazines do suck,” she said, laughing.
“Yeah, I bet they do. Everyone takes the good ones home. Let me see what else is around to read.”
That was an example of a real encounter between a nurse and a visitor—a visitor who had been reported many times as being a hard case. Usually, nurses just kept quiet when she was in the room, not addressing her at all. Some of them even wore stern expressions, while getting in and out fast, spending as little time as possible with the patient. Others, tried to kill her with kindness, but just ended up being laughed at or dismissed.
What made this nurses’ encounter different was that she began with a Universal Greeting. Then she Empathized with the woman’s situation. Then she asked questions to Clarify if there was anything wrong or if she had an unmet need. Then she performed a modified Paraphrase, even though she didn’t have much to work with, by stating, “I can see you’re upset about something.” Finally she Summarized by saying, “I just want you to know I’m here for you, if you need anything.” By going Beyond Active Listening, we can get to the real meaning of what people are saying. We can also open an opportunity to set limits on unsafe or anti-therapeutic behaviors. Most of all, we can begin to set a Social Contract that is compatible with healthy outcomes and incompatible with violent ones.





.png)