Enjoy this excerpt from one of our published books.
Chapter 10
Good Doc, Bad Doc:
Point of Impact Crisis Intervention
“A gentle answer turns away wrath, but a harsh word stirs up anger.”
-Proverbs 15:1
The dispatch center advised all units that a combative patient had just arrived at the emergency department via ambulance. I was the security supervisor on duty and responded from another building across campus. The rest of the security team was closer, all were experienced and well trained so I wasn’t overly concerned, during the drive over. By the time I arrived, I could already hear a commotion coming from the exam room where the patient had been wheeled in. When I poked my head in I saw a tall, young, athletic man spitting, cursing, and struggling against the EMTs’ tie-on cloth restraints.
The patient had taken an overdose of prescription medications and alcohol. He was also very strong and obviously feeling no pain. The EMTs had “packaged” him on their gurney in the swimmer’s position, with one hand tied above his head in an effort to restrict his mobility. The swimmer’s position isn’t the safest position for a patients’ body or psychiatric well being, making it inappropriate for hospital use. Although medical-surgical cloth restraints are commonly used in hospitals for combative patients, we needed to get them off of him.
Medical-surgical type cloth restraints are fine for temporality immobilizing the arm of a confused patient, who is unconsciously pulling at an I.V. line or scratching a wound site; but they are unpadded, rough in texture, and ill-fitting, making them hard on a combative patients’ circulation and skin integrity. We also needed to get both of his arms down at his side, as it makes a patient feel less vulnerable, especially if they have a history of violent or sexual trauma. It also places the patient in the optimal position to provide care and reduces strain on their muscles and joints. Therefore, the security team was preparing to transfer him to a hospital gurney and apply a five-point restraint kit specifically designed for combative hospital patients.
They were doing a nice job and had enough help, so I simply stood by, ready if needed.
Suddenly, a young resident physician walked in, while the nurses quietly prepared their I.V. lines and the security officers deftly continued stabilizing the combative patient. “Now you knock that off right now!” she shouted. “We’re trying to help you, so just lay there and be quiet!”
The patient took a few seconds to process what the young physician had just said. Then suddenly, he exploded. “F*** you, you f***ing stupid b****!” he shouted. Since the security team was in the middle of a transfer to the restraint kit, he managed to free one leg and kick over an I.V. pump. He thrashed and kicked wildly and the security team had to manually stabilize the patient, while the nurses froze or backed away. Just as I stepped forward to help, the curtains to the exam room flung open. An older surgeon passing by overheard the commotion and decided to see if he could help. He asked at the nurses’ station for the patient’s chief complaint and his name. What he did next was truly remarkable. As soon as he entered the room, he asked, “Who doesn’t need to be in here right now?” He didn’t have to ask twice, because every nurse and the young resident stepped out of the room immediately. Then he switched off the overhead examination lights and swung them out of the way. Then he said to all of us on the security team, “Okay guys, just stay quiet and I’ll do all the talking.” While we continued to apply the restraint kit, the doctor began to speak directly to the patient.
“Hello John,” he said. “I’m Dr. Washington.” The doctor spoke in a normal volume. He also spoke slowly and clearly, using a calm and reassuring tone. As he spoke, I think everyone on the security team started to feel their own tension diminish. After a brief pause, he continued talking to the patient who was still struggling and cursing. “John, you are in the hospital. You took too many pills.” The doctor paused again, giving time for the patient to cognitively process this new information—information that was obvious to everyone, except perhaps the patient himself. “John, we have to help you or you will get very sick,” he continued. “Please stop fighting and let us help you. You are safe with me here. I promise.”
At that point, you could hear the patient out-gas with a large exhale, as the tension fell away from his body. At each step, the doctor coached the patient into submission. “John, we are going to put these around your wrists to keep you still. We have to work fast, so please don’t struggle.” At that, he nodded to signal us to continue applying the restrain kit.
Dr. Washington and the patient started to have a conversation, while the nurses were slowly reintroduced into the scene. “This nurse is going to poke your arm because we need to get some medicine in you fast. Please hold still.” If the nurses and security officers were too loud or talking unnecessarily, he would “shush” us, reminding us to keep down the chatter. Soon, the patient was stable, being lavaged, and supported by his family.
When Dr. Washington turned to leave, I followed him. “Doc, you have a second?” I asked.
“Sure,” he replied.
“That was nice work in there. Thanks for your help.”
“No problem, glad I could help,” he replied.
“You should teach that technique to the doctors in training.
Where did you learn it?” I asked.
“It comes with experience. I’m not sure you can teach it,” he replied.
“That’s too bad,” I said, “because if you could teach it, these other doctors wouldn’t have to wait twenty years to learn it.” With that he nodded, smiled, and left.
Over the years I’ve seen scores of Crisis Interventions. Sadly, most of them ended badly. One thing I’ve learned is that natural language is disastrous. None of us really know what to do in a crisis, unless we’re trained or smart enough to learn from experience. That is, if we are lucky enough to learn from experience before getting hurt. Good training takes others’ experience and transfers it to someone else. We can only accomplish that through instructor led, experiential, scenario-based training.
I’ve been trained in several different types of Crisis Intervention techniques and “service recovery” models that either fell flat on their face when I needed them most or even made things worse! It’s true that human behavior is too unpredictable for all communications techniques to work in every case and on every person. That said, perhaps a method could be devised that is reliable enough and flexible enough to work on most people under most circumstances.
When customers, clients, and patients are wronged, we need to quickly repair that professional relationship. Sometimes we make mistakes and if we want to keep our customers, we better get good at making amends. One of the more common models of service recovery is the LEAD model. LEAD stands for Listen, Empathize, Apologize, and Do something. The first three words in the acronym are the same, no matter where you find them. In some places, the D might stand for “Deliver” or “Do the right thing”. In service recovery situations, it really works! LEAD is used everywhere from hospitals to airlines and it gets results. Fewer complaints and fewer lost clients. But if LEAD is the only trick in your bag, what are the possible consequences? Imagine the following situation.
A patient is yelling and cursing in his room, about his television going out and throws a bedpan out into the hallway. His nurse runs to the room to see what’s wrong. Armed with her LEAD training, she’s confident she can handle the situation.
LISTEN: “Mr. Gordon, what’s the matter?”
“My TV went out, g******it!” says the patient.
EMPATHIZE: “That’s awful. You must be bored to death.”
“If I don’t get a TV in here right now I’m going to sue!”
APOLOGIZE: “I’m sorry Mr. Gordon. I’ll call right away.”
“You better. I’ve had it with this f***ing hospital.”
DELIVER: “Can I get you a snack or some more coffee
while you wait?”
“Just tell them a**holes to hurry the f*** up with my TV!”
In this scenario, all of the elements of LEAD were applied, but what did it accomplish? On the surface it appears that it only accomplished one thing. It trained the patient to curse and yell at his nurse whenever he wants something, because in this hospital yelling and cursing gets results.
Using the 'Beyond Active Listening' Skill
Again, LEAD is a good service recovery model. People have the right to complain and get angry when things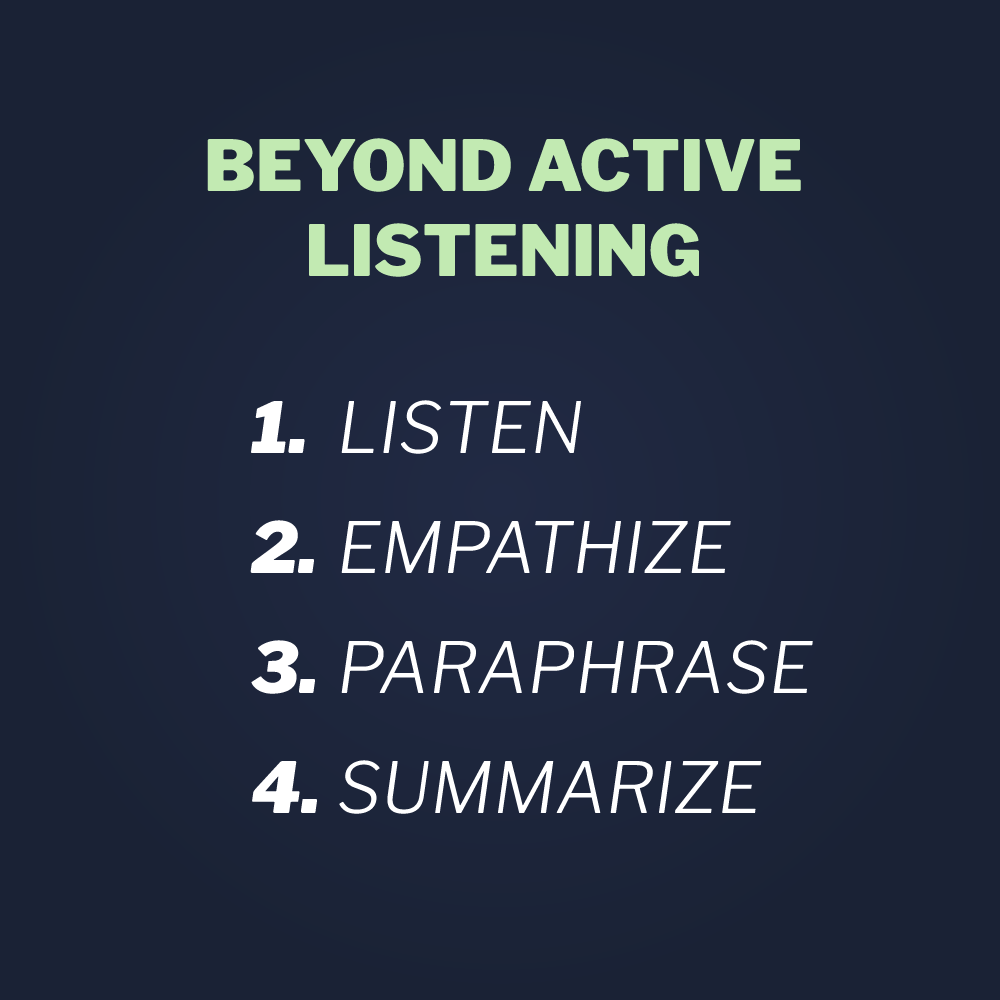 go badly. But they don’t have the right to engage in the gateway behaviors that lead to violence. By training providers to use Beyond Active Listening, we have much more flexibility, including the ability to set limits on gateway behavior.
go badly. But they don’t have the right to engage in the gateway behaviors that lead to violence. By training providers to use Beyond Active Listening, we have much more flexibility, including the ability to set limits on gateway behavior.
LISTEN: “Mr. Gordon, what’s the matter?”
“My TV went out, g******it!” says the patient.
EMPATHIZE: “I heard you all the way down the hallway.
I can hear you are upset. I know it’s been a rough day for you,” replied the nurse.
“Listen, b***h, this is bulls***. If I don’t get a TV in here right now, I’m going to sue this f***ing place!”
PARAPHRASE: “So you’re saying you are this angry and
threw a bed pan out in the hall because your TV isn’t working?” asked the nurse.
“No, d***it. Not just that. My leg hurts like hell and you won’t give me any more meds!” replied the patient.
SUMMARIZE: “Okay, Mr. Gordon. I’m glad you said some
thing. Your doctor said you are maxed out on your usual pain meds for today. But there are other things we might be able to try. I’ll call her and see what she says, but please stop yelling, cursing and throwing things.
I want to help you and I will. But you are frightening the other patients. There are kids and elderly people around. Can you work with me?”
“Yeah, I’m sorry,” replied the patient.
It’s okay, Mr. Gordon. I know you’re hurting. Let me go try and do something to help. I’ll be back as soon as I can. In the meantime, I’ll have someone bring you an icepack and we can also try to reposition you a little.”
Communication models will often fail if they are inflexible. Inflexible in the sense that they fail to mine for important information, set limits on unwanted behaviors, and formulate care plans and safety plans for moving forward. Also, communication skills aren’t just a series of steps; they are psychomotor skills that must be developed through training.
Crisis Intervention Strategies
In healthcare, law enforcement, and any human service work, we don’t just deal with dissatisfied customers. We deal with people in genuine crisis and those suffering from mental illness. There are times when people will exhibit gateway behaviors when in psychiatric crisis. On these occasions, we need to focus on the crisis and the behavior. Just as in the example at the beginning of this chapter. So what exactly did the surgeon do in the former example? The first thing he did was, reduce stimulation.
People in crisis act-out for a reason—not because of a diagnosis. This is also true of the patient with the broken television. Though his broken television may have been the last straw, the real reason he acted-out was because of his pain. This is a very common scenario in medicine. But the man in restraints acted-out because of the ingestion of narcotics and alcohol, so how did the surgeon get to the root of his problem? First we have to manage the sources of stimulation and frustration that all people in crisis have in common. The first of these commonalities is external stimulation.
The primary sources of external stimulation are light, sound, and the human presence. The first thing the surgeon did was to remove all unnecessary people from the room. He allowed the security team to stay because they were essential for the safety of the patient and himself. That said, he managed their presence by instructing them not to talk. This is the one voice concept.
Healthcare is a labor-intensive profession. Anyone who has been to a cardiac code call, or “code blue” as it’s commonly referred to, understands that. I’ve seen as many as twenty or more people crammed into a small patient room during a medical emergency with doctors, nurses, respiratory techs, and others all talking at once. I’ve also heard doctors struggling sometimes to get things under control by yelling something like, “Everyone just shut up!” Though that usually works, hearing doctors struggle to maintain order during a medical emergency is not very reassuring to the patient, the staff, and especially any family members within earshot. By training everyone to use the one voice command, we can restore voice discipline at the scene quickly, effectively, and professionally.
The human voice is one of the strongest forms of external stimulation. One voice equals communication. Two voices is just noise. Three voices equal chaos that is just another source of adrenaline to a subject in crisis. People in crisis abhor strange voices and sound. Unfortunately, healthcare providers and first responders hate silence. We all want to talk because we all want to help. The one voice command is a tool we can use at the scene to restore voice discipline in these situations as well. If everyone was trained in the one voice concept, it’s possible that the surgeon in the example may not have even needed to restore voice discipline, because everyone would have already understood that dynamic. But at very least, by stating loudly and clearly “One voice!” he could have accomplished the same goal.
He also removed unnecessary harsh lighting, by moving the examination lights out of the way and turning down the remaining lights — another way to reduce stimulation. We don’t need to have things dark, but lowering lights to a safe level is an effective tactic.
What he also did was separate and support the patient. Too many people at the scene, unnecessarily providing stimulation to a patient, is a common problem. By removing non-essential personnel, he managed that problem. Often, when people are in crisis, we need support for our own safety, but having support staff out of sight can go a long way to calming subjects down. With that in mind, he kept the security team on hand but restored voice discipline at the same time.
He also adapted communication. People tend to talk too fast and too loudly during a crisis. He spoke in a normal volume and soothing tone of voice. When people are loud our natural inclination is to match their tone and volume. Again, all behavior equalizes. Providers need to model the behavior we want to see. Crisis intervention expert Daniel Vega referred to this method as “reverse yelling”. When people are being loud we need to get quieter, even at times getting very quiet so they can follow us down to a calmer state of mind.
The surgeon also adapted his communication by stating the obvious to his patient. People in altered states of consciousness and others who might have brain-based disorders such as autism or Alzheimer’s syndrome, may struggle with understanding their circumstances. By telling his patient that he was in a hospital and that he had ingested pills and alcohol, helped fill in the blanks. He also spoke in short, direct sentences. He used his name frequently so he understood clearly that he was addressing him and not someone else.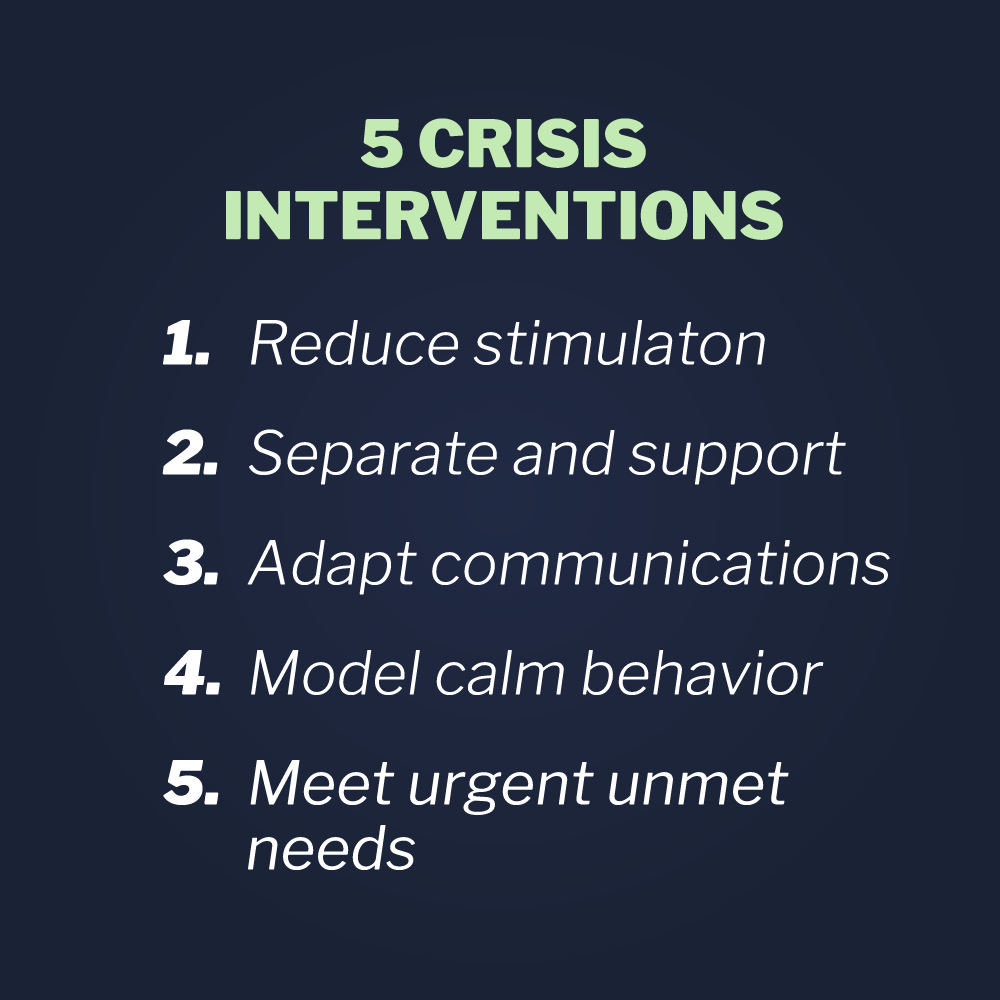
Meeting urgent unmet needs is another technique that can normalize people in crisis. I’ve seen all sorts of behaviors stabilize after meeting just basic human needs such as toileting, hunger, or thirst. I’ve seen biting and spitting behaviors disappear after just giving a non-verbal patient a cup of water.
These five tactics: reduce stimulation, separate and support, adapt communication, model calm behavior and meet urgent unmet needs are tactics that complete the skill set Vistelar calls Crisis Interventions. In an age when brain-based disorders are growing in unprecedented numbers, providers will need to become more proficient in such a skill set, which requires a commitment to training and education for providers.
To meet patient needs, think creatively
Human conflict is always a concern in the practice of healthcare, not only when serving patients who have brain-based disorders or psychiatric conditions, but for all patients experiencing a medical emergency or chronic medical condition. Limits on time and even space in medical facilities often ensure that conflict will occur, especially if policies are too rigid and providers too inflexible. Often we have to think outside the box to better serve patients and prevent conflict.
A woman with a severe headache presented at an emergency department, seeking help to manage her pain. None of her routine medications or anything she had tried was helping. As luck would have it, her headache flared up on a Friday afternoon. Now, over 24 hours later on a Saturday night, help from her family doctor was unavailable. Having suffered from severe and debilitating headaches for years, on rare occasions she had no choice but to seek help at an emergency room. This was another one of those nights.
Sometimes her headaches could last for days and the pain could be unbearable. Her headaches were more than a condition — they were an affliction; an affliction that had ruined her career, impoverished her life, and threatened her future. Over the years they had strained and even severed many of her relationships with family and friends.
Ultimately, they were at the root of a profound depression that had left her feeling hopeless and wrestling with thoughts of suicide. Still, that Saturday night she had enough hope left for one thing. She hoped for enough relief from her pain to eat without vomiting and sleep for a few undisturbed hours.
She had been through the E.R. process enough times to know what to expect. Depending on whom she got as a triage nurse, she would be treated with dignity and shown respect or treated like a drug addict. And depending solely on luck again, she hoped to draw a physician who would treat her with compassion and not suspicion. She’d been around the block enough to know that drug seekers are an issue at emergency rooms and that one of the symptoms they presented with was headaches. That is why she rarely sought help there. But this was just one of those nights when she just had to take that chance.
The waiting room was busy — crammed with patients, families and children. The television was blaring and the line was long. The bright florescent lights caused her to shield her eyes with her hands. Weak from the pain and an inability to eat, she could barely stand causing her to lean against the counter as she waited her turn at triage. It was all too familiar. She was in an environment that she would avoid under most circumstances, brightly lit, busy, and noisy. But she had to endure it if she was to take a chance at getting some help.
The triage nurse was obviously flustered, as she had been working diligently to cut down the line that kept pushing through the door. After checking in the woman asked, “Do you have somewhere I can wait that isn’t so bright and noisy?”
“Sorry, you’ll have to wait in the waiting room like everyone else,” replied the nurse.
“How long do you think I will have to wait?” asked the woman.
“We have to take patients based on how sick they are, Ma’am, not on when they arrive,” she replied, the implication being that her headache wasn’t a medical priority.
“I understand that, but can you give me some idea on how long?” she asked.
“At least a couple hours,” replied the nurse, tersely.
With that, she walked into the crowded waiting area. She tried to find an isolated corner, but there weren’t any. She found a seat and sat with her head in her hands, covering her eyes. The blaring of the television and the laughter of children cut through her brain like an ice pick. She wished she had asked for a basin in case she needed to vomit as she felt waves of nausea washing through her stomach. Just then there was a commotion in the triage line.
“I’m not waiting in the f***ing waiting room! I’m sick!”
“I understand that sir, but we are very busy,” replied the nurse. “This is f***ing ridiculous!” he said. “I want to see a doctor
right now!”
After a few more exchanges, she noticed a nurse rush forward from the back and escort the angry man back to an exam room. What she had witnessed was a familiar pattern in Emergency Department waiting rooms. Cause a scene or threaten the staff, and you won’t have to wait like everyone else. The woman simply bowed her head and wept into her hands.
Conclusion
Healthcare workers are decent and compassionate people. The job they do is tough, both physically and emotionally. Stories like the one above are an exception in some facilities but routine in far too many others. When we train hospital staff to treat everyone with dignity by showing them respect, they not only learn to serve patients better, but they learn to care for themselves and each other better. And when we train to set the tone for how we deliver care, in a way that is caring and inclusive for all, we can prevent anti-social and violent behavior, instead of reinforcing and encouraging it.
Thank you for reading this book. I hope it gave you some tools that you can use to keep safe and be confident in conflict. The principles of violence recognition and response espoused herein cannot bear fruit without forward thinking and risk taking by healthcare providers and public safety professionals like Mike Thiel, the Director of Security at Children’s Hospital of Wisconsin. None of them could have been developed or put into practice without the guidance of violence prevention and public safety experts like Bob Willis, Gary Klugiewicz, and Dave Young from Vistelar. The programs they instituted and the training they developed have had dramatic and lasting effects on the levels of violence experienced by the providers whose professional lives they have intersected. I join Mike, Bob, Gary and Dave in wishing every healthcare professional who reads this book, a long, happy and safe career.



.png?width=150&height=150&name=Podcasts-%20Newsletter%20Featured%20Image%20Template%20(1).png)