“Vistelar’s Training Demonstrates a Positive Impact on Behavioral Health Professionals ” - Episode 20
Host: Allen Oelschlaeger
Guests: Dr. Danielle Romaine Dagenhardt, Matt Richie, Ph.D.
Subscribe to our podcast on Apple Podcasts, Stitcher, Google Play or YouTube.
On this episode, Allen talks to two of the researchers who conducted a study of the effectiveness of Vistelar’s training at the Milwaukee County Behavioral Health Division (MCBHD). They spent countless hours observing as the majority of MCBHD’s staff received end-user training that ranged from verbal non-escalation/de-escalation to team stabilization tactics. From environmental services to physicians, participants from across the organization participated in the training and ultimately the study.
The data gathered, through surveys, focus groups, and quantitative data showed an overall positive impact on various concerns that prompted the training in the first place. The training showed some of the following benefits:
- Reduced role conflict between different staff members
- Improved individuals’ conflict resolution skills
- Increased safety or perceptions of safety while at work, reduce burnout and turnove
For more information about this research study, or to download the various reports, click here.
Allen: Good afternoon, Matt and Danielle. It’s great to have you on our podcast. Before we get started, Danielle, why don’t you just do a quick intro of yourself and then we’ll do that with Matt. And then we’ll talk about this study.
Danielle: Sure. My name is Danielle Romaine Dagenhardt and I’m an Assistant Professor in Criminal Justice and Criminology at University of Wisconsin, Milwaukee. And I was a co-investigator on this evaluation of the Milwaukee County, Behavioral Health Division gatekeeper training.
Allen: Cool. I wondered if co-investigator what a great title. Go ahead, Matt,
Matt: Matt Richie. I’m an Assistant Professor at the Department of Criminal Justice at the University of Wisconsin, Oshkosh and I serve as a research assistant throughout the project.
Allen: Yeah and just quickly let the audience know about how University of Wisconsin works? So you’re from two different University of Wisconsin schools, but how many are there in the state? Like a lot?
Matt: That’s a good question.
Allen: 10 something, right?
Matt: I was actually at the University of Wisconsin, Milwaukee when we did this study while I was finishing up my graduate school.
MCBHD Conflict Resolution Training
Allen: I don’t know. I taught, not criminal justice, not without a PhD, but I taught at a Whitewater for three years. I think this whole professor thing is so cool. I’m very proud of you guys to be doing this. Okay. So we did this study and lets look back to 2017. Do you remember how we got started in this and what kicked this off? It was Tina, right? Go ahead.
Danielle: Yeah, it was, Tina was approached by someone from Vistelar. I think it was Bill Singleton, that they were planning on partnering with Milwaukee County BHD to do this new training on conflict resolution, escalation and de-escalation. They wanted to find an outside evaluator to see whether or not the program actually works at meeting its goals.
Allen: Yeah. So effectively it’d be Milwaukee County Behavioral Health Division, which is our local county based behavioral health facility contracted with University of Wisconsin, Milwaukee to do this study.
Danielle: Yes.
Allen: And both of you were involved from the beginning?
Danielle: I was involved from relatively the beginning. I was not privy to the initial conversations, but once it seemed like this was something that could be funded and could be a good evaluation. Tina Freiberger approached me for some assistance on working on the project.
Allen: And then Matt, you got involved when?
Matt: I knew about the project just in conversations, but I think I came in when we started evaluating the process of it, sort of shadowing trainings and seeing what the training looked like and how it worked and sort of a fidelity evaluation there.
Allen: Yeah. So you remember what the original goals Danielle, when it was first?
Danielle: Yeah, they had quite a few goals that they wanted to accomplish, specifically Milwaukee County BHD. They really wanted to reduce role conflict between different staff members, as well as improve individuals’ conflict resolution skills. They wanted to increase safety or perceptions of safety while at work, reduce burnout and turnover, which I think is something that’s pretty common in organizations that provide behavioral health and mental health services. They also wanted to increase individuals’ perceptions of patients, particularly those that work with patients almost like in a direct care format, so if they work on the unit with patients.
Lateral Violence
Allen: So do you remember, we’ve talked about this a lot is the difference between when we talk about conflict and where we’re then within our organization and you’re in a mental health hospital, obviously you would imagine that most of the conflict is with patients, but the first thing you talked about was conflict within the departments, right? Is that kind of between each other?
Danielle: Right. Conflict between each other. This could be things like security officers and nurses having conflict about what to do if there’s a crisis with a patient. Who should take the lead on ensuring safety of the patient, restraining a patient, things like that. It can even include just general conflict between coworkers like rolling your eyes or making a sarcastic remark.
Allen: Yeah. The term I should probably, this probably has been around for a long time, you guys know, but lateral violence. That’s a term I’ve only been introduced to here in the last year or two. Is that a term that’s been around for a long time?
Danielle: I think it’s been around for about 20 years now from the first kind of study that I think published a scale, the concept, but going in terms of knowing that terminology. So usually it’s a lateral violence or horizontal violence, which is just basically lateral violence.
Allen: Lateral meaning individuals having conflict with each other within an organization rather than with the customer or the patient or the student or whatever, right?
Danielle: Yeah. Yep. Conflict between people that work together.
Allen: When you think back was it kind of an equal thing between the dealing with the patients or was it lateral violence, or was it more focused on one versus the other, remember?
Danielle: I think it was relatively, even in terms of the goals that they had, they were really concerned about role conflict, particularly that staff really didn’t know whose position it was to make decisions in crises. Being asked to do one thing, but policies and procedures might tell you to do something else and really knowing what their job is in a situation, but really also making sure that staff have better perceptions of patients and have empathy. So I think it’s definitely a dual emphasis.
Allen: It was the methods. This got to be a pretty comprehensive study. This wasn’t just like a little survey thing you guys were, I mean, there was a whole bunch of elements and you stayed with the group for what, a couple of years?
Danielle: Yeah. We actually did a longer follow up then what I think you typically see. We did a baseline survey before individuals got the training and then we followed them up one month after the training, one year after the training, and two years after the training to see whether or not people’s perceptions change long-term or was it more of a short-term change.
Allen: Very cool. Was it just surveys or did you do interviews and focus groups? How did you collect the data from them?
Danielle: We did mainly surveys, but we also did some focus groups that Matt led with two different groups of staff. We did one that was direct care individuals, so nurses and nursing assistants, and then one of that was non-direct care staff. I think most of them were working in a community engagement kind of capacity.
Allen: Matt, my experience has been that human interaction surveys stop, you learn more than what you can get out of a written survey offer.
Feedback from training participants
Matt: Yeah. I think that’s initially why I volunteered to do the focus groups. Cause I think staff are usually pretty vocal when you ask them the right question. I thought that this was a group of people that seemed frustrated. They seemed anxious about what they could and couldn’t do in their own work. So I asked them how they felt about the training. I think a lot of it was a relief, there was less of this like mental handcuff on what they could do. A lot of them, I thought after not only the verbal and the physical training, but there was a sense of empowerment that they understood what they were supposed to do in different scenarios.
Matt: I think through that, there was more collaboration, which I think would have led to a reduction in lateral violence because you weren’t worried about someone not covering you because they’d all been trained the same way. It was more of a team mentality. I think, at least certainly with the direct care staff, I thought that they really bonded over this sense of we know what we can do. We know we shouldn’t do, and now we can be more effective and keep ourselves safe. I think that’s one of the stories I remember hearing was a staff member had been assaulted at work and it was clear that nothing had been done to prevent that from other coworkers. I think after the training, it was like, we know what we have to do when we see that starting so we can bring them down earlier.
Allen: You did those interviews, when? Was that right after the training?
Matt: It would have been a couple of months after the training and sort of had time to synthesize the material and sort of get comfortable in that space. So I was impressed that they had, like the training had ended and then we’d had sort of not train the trainer episodes, but they’d sort of decided to work on these things themselves. Like they had the manual still and they could sort of check in with one another on whether it be universal greening or proxemics as sort of reassess and sort of reteach each other, these skills over time, which I think is something that is rare because we’ve all taken trainings at work or whatever. A lot of times the information goes in one ear and out the other, and you’re just trying to get the training done. It seems like this one had certainly more staying power with the staff.
Allen: That’s one of the things that the one and done training of just going in and doing a class and everybody leaves and they go, yeah, whatever. But in this case I think there, and I remember the name, we call them champions of people that were quite interested in it. And then I think some of those people got some additional training and then they went back to their staff over time and continued to reinforce the main points. It wasn’t a formal training thing. It was more of an influence and just championing, being an advocate for it within our department or a floor. Right? Do I have that right?
Danielle: Yeah. They also attended the newer trainings for any new hires and anyone that had already [crosstalk 00:11:24]. Yep. So they were able to sit at some of the different tables and kind of help teach and coach people that are fresh.
Allen: Well, I know there’s a huge opportunity for this because it’s where we have the opportunity to touch every single person in the organization. I’ll just do a quick summary. You can guys can elaborate, but what I remember was we actually went in and trained everybody with a one-day program initially. That was all the frontline staff, gatekeepers, direct staff, whatever. Then we went back and trained just the direct care staff with another two days of training. Is that right?
Danielle: Correct. I think there was a few people that it took a little bit longer for their scheduling to get trained, but everyone was trained on the gatekeeper training. Then that more intensive training that Matt was talking about, direct care staff, got over a two day period.
Allen: The first day was largely verbal skills. Then the second two days were mostly physical skills. Was that the way it was structured?
Matt: Yeah. I think the first day is mostly sort of that verbal communicative skills. Then for the direct care staff, there are unfortunately this is where physical tactics are necessary. I think that was a real source of anxiety for the staff initially, because the report about the restraints had come out and there were new rules about that and how you had to handle patients like that. I think that the staff were frankly nervous about what they could/couldn’t do to restrain someone who’s having a problem. I think having the trainer sort of go in and say, this is how we’ve trained you. So this is what’s acceptable. Hold it sort of removes the liability from you personally. And I think, I mean, you could hear like a relief in the room at these times. This would be like, okay, now we like we know, and I think they would practice that later because it is a lot of it’s body mechanics.
Matt: So you’re not, I think that’s what makes it a safe strategy is that you don’t have to be a linebacker to do a lot of these things. It’s mostly body mechanics and weight distribution, and it allows you to keep you safer and it’s an approved tactic by your employer, so you can’t be held liable for it. I think that was for the direct care staff who are seeing these things much more often than the non-direct care staff that made everybody feel less anxious and more comfortable in their sort of direct care units, because it does happen that you need to go hands-on with someone and being mindful of how that situations playing out, where you’re at. I think the staff just felt so much better about that. With all of the training combined, it seemed like they felt better equipped to do their jobs.
Allen: I don’t know if you guys were there, I remember one story that, where there was I think a very small woman, maybe five, two, or whatever. And there was the patient that was all mocked up, but it was like a 250 or 300 pound man. They were able to hold the guy down using our tactics. Were you part of that one where the five to just, it’s basically what you described, Matt, very feeling a sense of empowerment of, wow, we can actually do this.
Balancing Verbal & Physical Care Tactics to keep everyone safe
Matt: I don’t know that I remember that exact instance, but I do remember a woman of a similar size holding down someone very large. I think that’s in the body mechanics. How can you use your weight and their weight against them to sort of quell the situation? A lot of the two day, because it is longer because the tactics do require some body mechanics and sort of memory. I think a lot of it, don’t talk enough about is the verbal stuff. Just like how critical, we can all say that verbal is our first line of defense, but I think that training taught them that it’s the first through the 10th. We’re going to use this as long as we have to and it’s not about meeting someone’s level. It’s about bringing them down to a more calm and cool level, because then we can, we can get more done and we don’t have to be physical.
Matt: But I do think the physical tactics were something that smaller staff, they felt better and they felt more comfortable in that space because it wasn’t this, they could do it by themselves. And I think that was a big piece for them.
Allen: Yeah. We were joking before we got on the recording here, but the two of you have probably, in the world of conflict management training, have probably sat through more of our training than anybody else in the planet. Cause you, as part of the study, you were actually in class for how many sessions? Like a lot, right?
Danielle: Yeah. I think it was about 20 sessions between the two of us.
Matt: I don’t want to teach it. I’ll let Gary and the rest of the team do that. But it’s there.
Allen: Yeah. Just quickly without going through. I mean, there’s a lot of, as everybody knows that’s been listening to this podcast, we address the entire spectrum of view and conflict now, which is what you’re describing. Right. All the way from the verbal stuff to crisis and the physical things or whatever, but just quickly, what would be a couple of things you remember from whatever that was four years ago that maybe you use in your personal life?
Danielle: Matt, you can go first.
Proxemics
Matt: Proxemics is always something I kept with me, I still have the card in my wallet because it was a way to sort of manage space, I think. And of course, like pre pandemic, I will think I was always sort of mindful of that 10/5/2 rule. Right. And I think not that I’m ever in any real danger in the classroom, but at least I’m able to sort of manage that space more effectively in case something like that would ever happen that I know at 10 feet, I’m cool. I know what to do at five, a little closer, a little more ramped up and at two we either start talking or find a different solution.
Matt: But the proxemics I think just cause it was so simple and it was something that didn’t take an extensive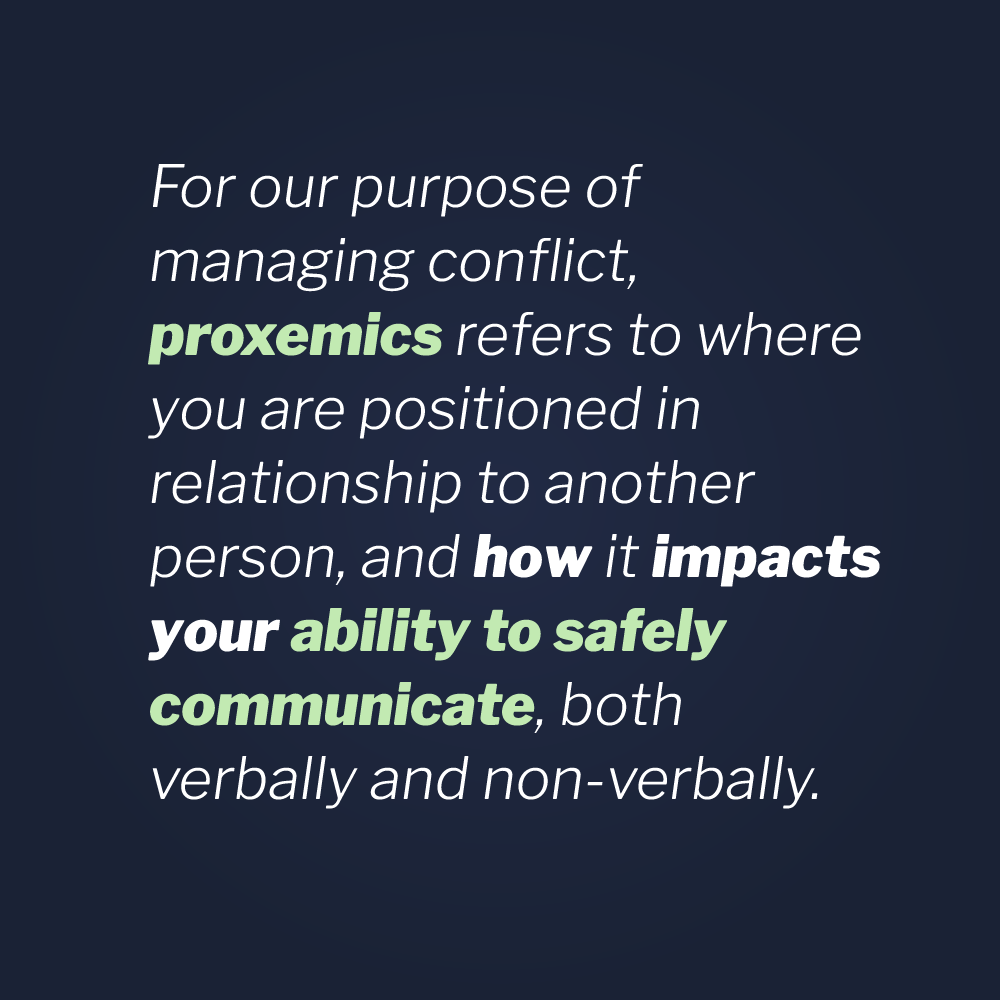 amount of training and it just seemed so effective because staff knew that they didn’t have to walk up to someone if they’re getting aggressive. They can keep their space and sort of allow that conflict to resolve itself in some instances, without escalating individuals, because I think the beauty of it is that it’s non escalation, not de-escalation, let’s start at nothing rather than bringing them back down.
amount of training and it just seemed so effective because staff knew that they didn’t have to walk up to someone if they’re getting aggressive. They can keep their space and sort of allow that conflict to resolve itself in some instances, without escalating individuals, because I think the beauty of it is that it’s non escalation, not de-escalation, let’s start at nothing rather than bringing them back down.
Allen: So Matt, this goes back a few years, but we did a lot of work with a group of shoplifters, the shoplifter, the loss prevention people that are in retail stores who have to deal with shoplifters. At the beginning of the class, we said, okay, well walk up and show us how you approach somebody that is shoplifting. They literally, I mean, these were people that had been doing this for five, ten years. It was their career and they literally would walk up with their hands in their pocket and get within two feet of the shoplifter and say, “well, sir, do you have something in your pocket that you shouldn’t have?”
Allen: Wait a minute here. Are you serious? It was like this is a wow moment of saying, no, why don’t you step back five feet, get your hands up and just be aware that something could happen here rather than just assume nothing’s going to happen.
Matt: No, I think that’s what people don’t always think about. I think there is always space if the person isn’t already elevated to sort of talk through whatever issue you have in the study I published last year, it looks at like how jail staff manage conflict in the jail. It’s just so much easier to use verbal than physical. Right. But I think like being mindful of space is so critical to even avoiding interpersonal conflict, avoiding your own risk to safety. I think that’s really where the 10/5/2 rule is, unfortunately, always in my head because of the days of this alert training I have at this point. But I do that.
Allen: Matt, is making the other person feel comfortable. If you need to stay safe, but you get too close and the other person who might be fine, but all of a sudden you’re two feet from them and they’re going, “Wow. they’re getting ramped up.” Danielle, what would you remember from four years ago?
Showtime Mindset & Redirection
Danielle: Yeah, I would say the Showtime mindset and redirect have really stuck with me. Sometimes there’s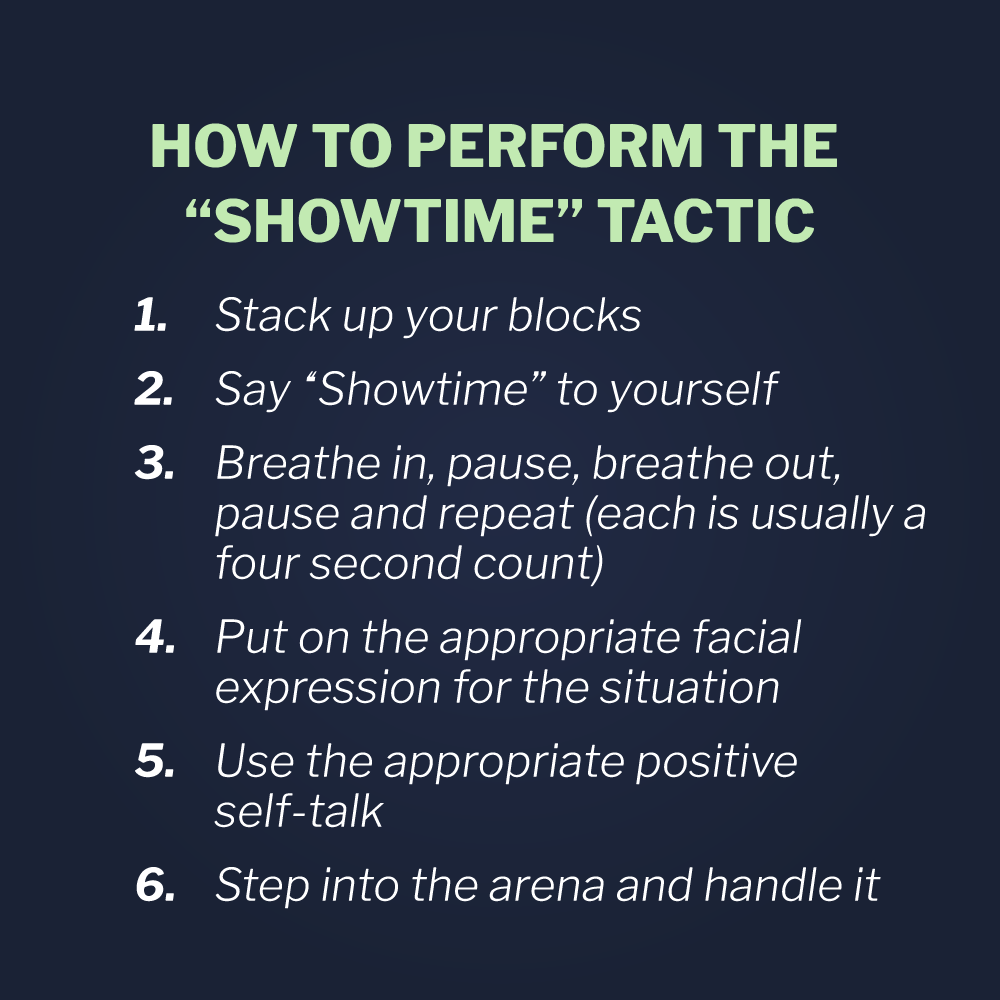 very stressful days and I think back to the Showtime mindset and having to go from one stressful situation into something else, having that pause, kind of grouping yourself, stepping on stage it’s Showtime has helped. I’m currently dealing with the soon to be one year old, so the redirect is very helpful to avoid tantrums.
very stressful days and I think back to the Showtime mindset and having to go from one stressful situation into something else, having that pause, kind of grouping yourself, stepping on stage it’s Showtime has helped. I’m currently dealing with the soon to be one year old, so the redirect is very helpful to avoid tantrums.
Allen: Big time. Yep. I used it with our kids all the time. Yeah. It’s very, very powerful. I think you guys know, I mean, in the early years we, we still do some of this, but we did a lot of anti-bullying training and that was the primary skill we taught to kids in grade school and middle school was the redirect of how do you deal with somebody who’s abusing you and bullying you and whatever. We won’t teach it here, but very, very powerful technique on how to just get out of that situation and still being respectful and letting the other person save face, but not have to deal with getting verbally abused, although the one year is not verbally abusing you quite yet.
Danielle: No, but it definitely saves from when something escalated from a little upset to a full-on meltdown, so it hasn’t used it yet.
Allen: So the results, there was some short-term results and then a year and then two years, and you had both quantitative stuff, actual real number kind of stuff. And then there was qualitative, there was a personal interview. Everybody that’s listening to this can have a chance to get the actual study, they’ll be able to download it. But what do you remember is kind of some of the highlights from the results?
Danielle: Yeah. One of the things that I think is really positive about the training is that people even up to two years after had better perceptions of how to keep themselves and others safe, whenever things could potentially increase in conflict and aggression. Another thing that I think is important to the training is that direct care employees really felt more confident in working with patients. They felt like there were less constraints from behavioral health division on providing appropriate care. But I think that kind of goes back to what Matt was talking about, where they felt like they now have the tools, the tools from the training reflect the policies and they don’t necessarily feel like their hands are tied if they have to engage with the patient physically to kind of deescalate the situation.
Allen: This confidence thing comes up all the time with us. We always think it’s going to reduce injuries. There’s going to be less conflict. There’s going to be less workman’s comp claims. There’s going to be better morale, whatever. But when we do our own surveys, it’s just that word, confidence, comes up a lot. It’s just feeling more confident to be able to be in a situation where conflict might occur and knowing that you know what to do, and you’re probably doing the right thing and you’re not going to get in trouble for it. I don’t know if you guys know, but it’s early on when we had to choose a title for the books we published. We selected Confidence in Conflict as the headline title for all our books.
Allen: Matt, what do you remember?
Matt: I think going back to what Danielle was saying, I think there’s just so much less ambiguity. I think that’s why people don’t get frustrated and nervous when they know the game and understand what A and B is. They’re not worried about it. I think being specific about what’s expected and what you can and can’t do, brings down that ambiguity, it makes people feel more comfortable, which is why I’m not. We did the focus groups shortly after the training and so it was still relatively fresh, but to see it, two years later that it hasn’t shifted isn’t surprising. I think there’s less ambiguity. They understand and it’s all uniform, like everybody got the same training and everyone knows the same tactics and they can all sort of speak the same language.
Matt: I think that approach almost has to be the approach you take when you’re dealing with any agency, is that everyone has to be aware of all the same tactics, all the same communication to make this be effective. I think BHD, I applaud them for really taking the deep dive here and implementing this program agency wide so that everyone is on the same page. I think putting new hires through a day to two-day training is no small ask, but I think their commitment to this new approach is sort of a non-escalation approach and keeping things uniform is something that I think can only help BHD and agencies that adopt this down the line. I think that’s really, that ambiguity is always, that was always what was most frustrating and the empowerment they got from the training. I mean, you could just see it in their eyes and hear their voices when the training was over. They were like, finally, I don’t feel like I’m trapped. I don’t feel in danger anymore. I feel like I can do my job effectively now.
Allen: Just for the audience, you say the term non escalation a few times here. I think everybody probably understands what that means, but that’s our terminology for preventing conflict. Doing all the stuff that you can do to keep things from ever escalating, rather than only thinking about de-escalation and crisis management. And what do I do if I get hurt or hit. The focus is let’s prevent this, so you never have to deal with it, but with the awareness that you still might have to deal with it, and then having the confidence that you know what to do, if it ever happens. So I, I just remember a lot of when I read the study, a lot of what I thought were kind of crazy numbers in terms of percentages were 93% some thought this, and 97% thought it was useful and you know, 91% said they continued to use the tactics. Is that normal or was that kind of a surprise?
Danielle: That was a surprise to me, in particular, that after two years of experiencing the training, that there was a pretty sizeable proportion of people that still utilize the training and the vast majority of the people that utilized it really did find that it was effective most of the time at either keeping something from escalating or deescalating something that might’ve already started to blossom as a conflict.
Allen: Yeah. Matt, your point about having a unified system that everybody has bought into, and they’re all getting the same training, the terminology, I think is a big part of that. Just knowing what to call things. Like Danielle, you talked about Showtime Mindset. We see that all the time. If everybody knows what Showtime Mindset is and we’re not going to teach it here, but it’s basically a mindset of saying step back, take a deep breath, get your facial expression right. It’s Showtime, it’s time you’re stepping on the stage. This is a performance. We’ve seen it in emergency departments where it’s literally somebody is maybe just getting a little bit escalated and it’s just somebody else can just look at them and say, “Hey, showtime” and they go, oh yeah, they get it immediately. And it’s just one word and it can change the whole nature of an interaction.
Allen: Your one-year-old will remember the Showtime.
Danielle: Yeah. He’ll also remember that I rarely it now [crosstalk 00:28:42] .
Allen: Yeah. When they’re under three and it’s you, Danielle, that need to yeah.
Danielle: Yeah. Then I’ll be told Showtime.
Allen: Hey Mom, Showtime.
What stands out about Vistelar's Training?
Allen: So what did I miss here? What else should we be talking about relative to the study and in terms of, and obviously you guys, you do research, right? This is just one of many studies. Is there anything else that makes us unique or stands out or whatever?
Danielle: Yeah. I think there are a lot of conflict training programs out there, and there is a decent amount of research on a lot of these programs, but the sheer kind of number of goals that they wanted to accomplish. And how many of those actually were met, not just about increasing confidence in skills, but decreasing burnout, decreasing turnover. I think that really speaks to the power of this training to go beyond just competence, but really affecting kind of the culture of the workplace and how people interact like the horizontal violence and having less role conflict.
Allen: Yeah. I remember that was when we got started, culture was a big word used that we need to modify/improve. I can’t remember what the goal was, but culture of just how people interact and kind of the whole fabric of how the place operates. I think we accomplished some of that. I mean, that’s a big goal, change of culture. I think they have seven, 800 employees. It’s that kind of number. So this is not a group of five people you’re changing a culture for, it’s a big organization.
Danielle: Yeah.
Matt: I thought that was a key piece because people that reduced ambiguity increased empowerment and you sort of saw them ushering new staff in the same way. It was like, this is how we do this, and this is what this means. And I think their initiative to really take their training and embed in their workplaces, in their units and then usher and sort of acclimate new staff to this was a big, it tells me that this is effective if only to make staff feel safer and feel more confident in their roles and it's staying power. I think that can’t be understated that so much of this is still around four years later.
Allen: Danielle, do you have another point? I was going to make just one thing I heard recently about behavioral health, but go ahead.
Danielle: Oh yeah, no, I was going to say it’s kind of hard to measure culture quantitatively, but I think the focus group information that Matt got really attested to a lot of staff feeling like the culture really has shifted towards more understanding between all staff, even not on the same unit and comfortable that someone else coming in. If they’re just walking through the unit or subbing that they all have each other’s back and know what to do if something happens.
Concluding Remarks
Allen: Yeah. I will share the comment I heard a couple months ago from a children’s hospital actually. And you know, this is a behavioral health hospital, so mental health patients and it’s children’s hospital that deals with kids and you think, friendly place and whatever, but she said the whole, in her opinion, entire health care environment now is shifting towards a behavioral health environment. There’s so much mental health, mental illness and issues with anxiety and whatever that all the principles that apply to that would be really, really crazy important within a mental health hospital or a behavioral health hospital, are now applying to pretty much any healthcare institution. Matt, with your experience in criminal justice and corrections it’s same issue as Gary says, you know, corrections they’re kind of the de facto mental health hospital now.
Matt: Yeah. Well, I think it was good to see when we did the study a couple of years ago, a different study and the recognition that we don’t have to fight everybody all the time. I think a lot of, I mean, we don’t hear about anything it’s usually good news, but we don’t hear about it, so we don’t find out about it. But I think this shift towards interpersonal skills being the first line of defense and then just like keeping at that until we’ve exhausted it is where certainly corrections and law enforcement is heading at this point because it’s too much physical work to be going hands on every time and it’s an immense amount of paperwork. I really think that if we’re going to be equitable in our treatment of the individuals we serve that we have to be more attuned to our interpersonal skills and less resorting to physical skills. Use of force, never photographs well, that’s a hat tip to Steve Brandon who says that all the time. But I think that is a demand from our communities to use more verbal initiatives and less physical.
Matt: I think that Vistelar training teaches them that that’s what’s most important and that the physical tactics take two days because they are more involved. But if you can talk someone out of being violent, you’re far better off than if you have to fight with them to not be violent.
Allen: Matt, I love your comment about paperwork. It’s one of my, every time you guys are both new with our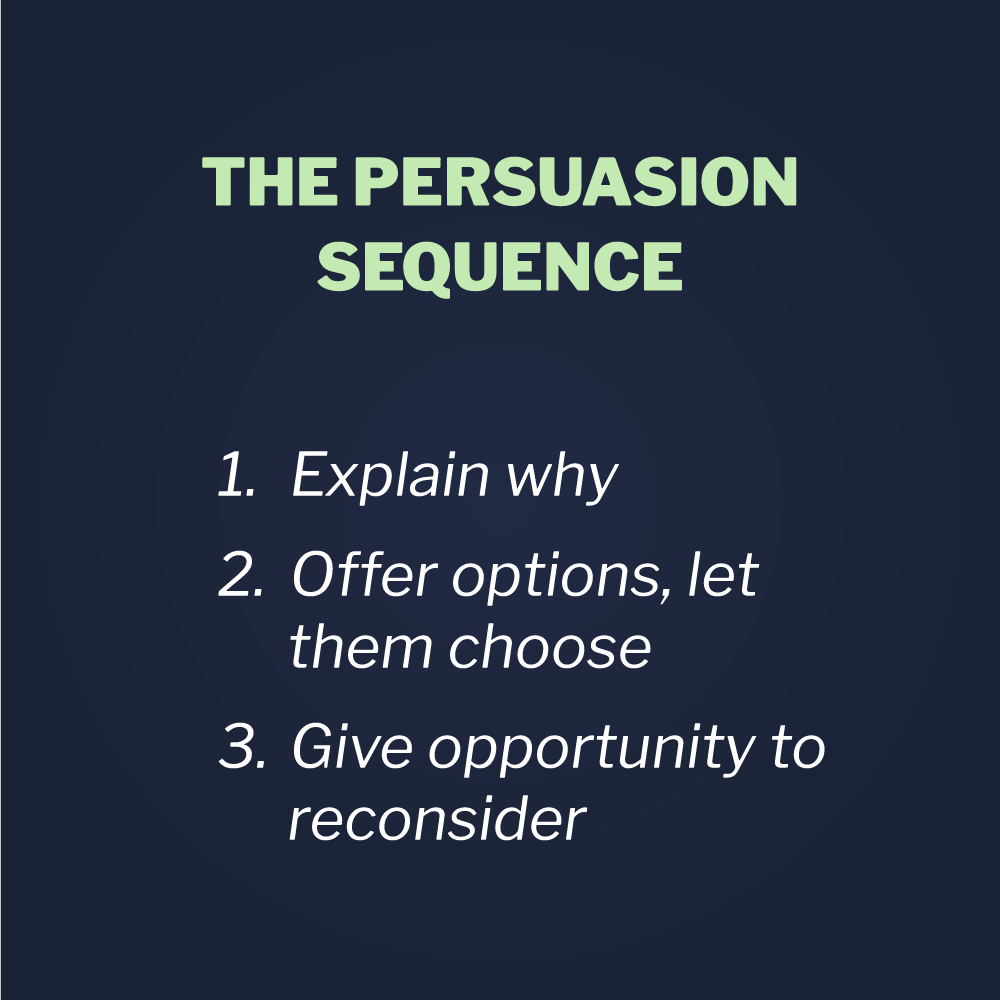 persuasion sequence. And the second step is to give people options, right? Here’s a good option. And then, oh, we got some bad options, but I just love it when police officers go, “you just can’t imagine the paperwork we’re going to have to go through here and how long that’s going to take.” And you really want to do that.
persuasion sequence. And the second step is to give people options, right? Here’s a good option. And then, oh, we got some bad options, but I just love it when police officers go, “you just can’t imagine the paperwork we’re going to have to go through here and how long that’s going to take.” And you really want to do that.
Matt: Right. Whatever it takes to deter future violence. I think if the paperwork will stop it, then I’m all for it. And I’m chatty. So I think I can talk in the most things, but I think it just seems like a safer route for everybody's role, the person who’s in need of help and the person trying to deliver help. I think it’s just an overall better route. And I hope we see more of it down the line. I think Vistelar really has an opportunity to promote this in different areas, behavioral health, law enforcement corrections. I think it’s a real promise there.
Allen: Yeah. Very cool. I, obviously, very much appreciate your time. I think the training started in September of 2017. Does that sound right? So this is two years and then there was kind of a follow-up report, right. Wasn’t there an initial report and then kind of a second where you actually got access to some of the hard data that you talked about, right?
Danielle: Yeah. So we first did a one month report, which would have been in, I think December of 2017, looking at just kind of one month changes. And then we did the final report of the survey and the focus group data. And then we also did a supplemental report on actual files of use of restraints and use of seclusion. That data also suggested that the training significantly reduced having to rely on those from the period before the training.
Allen: Yeah. Very cool. Well, appreciate your time. Thanks so much. And you’ll have a chance to hear all this here again once we get it all finalized and buttoned up and we’ll get you a copy of the file. So thanks.
Danielle: Cool.
Matt: Thanks for having me.
Allen: Take care.





.png)

