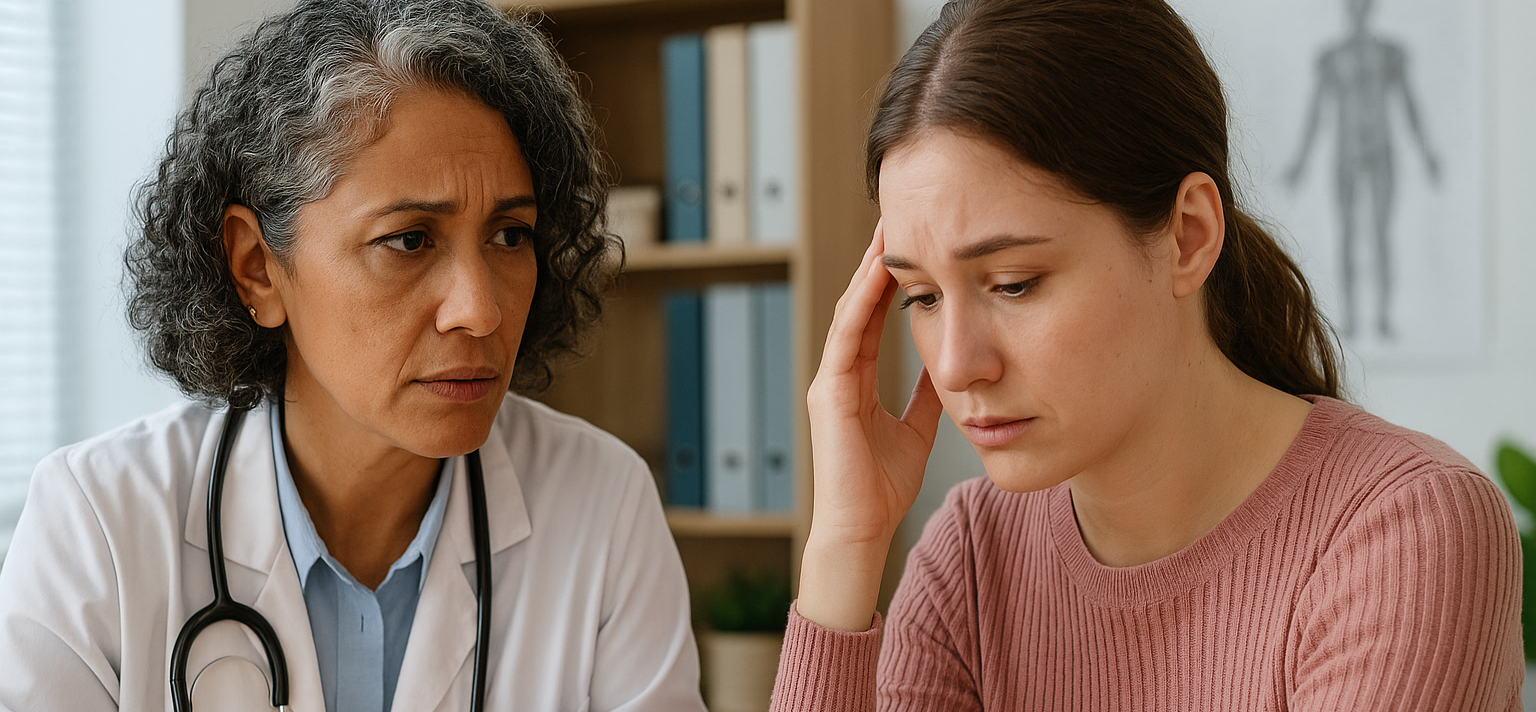
In healthcare settings, every interaction carries the potential to either heal or harm. Even a routine medical encounter can quickly transform from a healing opportunity into a re-traumatizing experience. As healthcare professionals, understanding trauma-informed communication isn't just beneficial—it's essential for providing compassionate, effective care that honors the dignity of every patient we serve.
Understanding the Trauma Landscape in Healthcare
Trauma doesn't discriminate. It crosses all demographics, affecting patients from every background, age group, and socioeconomic status. Yet many healthcare professionals remain unaware of how deeply trauma can influence a patient's behavior, responses, and ability to engage in their own care.
When patients enter our healthcare environments, they may be carrying invisible wounds from adverse childhood experiences, domestic violence, military service, medical trauma, or countless other sources. These experiences can create lasting neurobiological changes that affect how individuals perceive safety, process information, and respond to authority figures—including healthcare providers.
The Vistelar Approach: Building Bridges Through Empathy
Vistelar's conflict management principles offer a sophisticated framework for trauma-informed communication that goes far beyond simple courtesy. At its core, this approach recognizes that true empathy requires action, not just understanding.
The Four Steps of Empathetic Communication
- Use Curiosity to Understand Their Perspective. Begin every interaction by genuinely seeking to understand the patient's experience. Ask yourself: How would I feel if this were happening to a loved one? What might be driving their reactions? This curiosity should extend beyond emotions to encompass their thoughts, motivations, and concerns.
- Pay Attention to Non-Verbal Cues. Trauma often manifests in ways that extend beyond words. Watch for facial expressions that don't match verbal communication, changes in tone that signal distress, or body language that suggests hypervigilance or dissociation. These observations provide crucial information about a patient's emotional state and trauma responses.
- Ensure Appropriate Eye Contact. Eye contact can be particularly complex for trauma survivors. While maintaining appropriate eye contact demonstrates attention and respect, forced eye contact can feel threatening to someone who has experienced trauma. Allow patients to guide this interaction, respecting their comfort levels
- Take Action to Demonstrate Respect and Concern. This final step transforms empathy from a feeling into a tangible skill. Without concrete actions that show respect and demonstrate genuine concern, empathy remains merely an intention.
Trauma Responsiveness: Advanced Empathetic Practice
Vistelar's approach to trauma responsiveness provides a structured method for recognizing and responding to trauma's impact on current behaviors. This advanced form of empathy acknowledges that past emotional, sexual, or physical trauma can significantly influence how patients interact with healthcare providers and navigate medical environments.
Creating Safe Spaces Through Environmental Awareness
The physical environment plays a crucial role in trauma-informed care. Implementing Vistelar's environmental management principles can significantly reduce trauma triggers:
Reduce Stimulation:
- Respect personal boundaries and avoid crowding patients
- Move slowly and deliberately
- Soften lighting, reduce unnecessary noise, and speak softly
- Use “One Voice Communication.” As much as possible, ensure only one care provider speaks directly to the patient during interactions
Separate and Support:
- Limit unnecessary staff, visitors, and onlookers while maintaining appropriate safety measures
- When feasible, move to quieter, more private areas
- Connect patients with familiar staff members or appropriate support persons
Communication Strategies That Honor Trauma Experiences
The Power of Adapted Communication
When patients are experiencing cognitive challenges—whether from trauma activation, medical stress, or emotional overload—standard communication approaches often fail. Vistelar's adapted communication techniques provide practical alternatives:
Support Cognitive Focus:
- Use the patient's name frequently to build a connection and focus their attention
- Use short sentences and plain language
- Slow down your speech and maintain a calm tone
- Avoid “baby talk,” condescending or childish tone and language that can feel patronizing
Anticipate Processing Needs:
- Don't interrupt patients when they're speaking
- Avoid repeating yourself unnecessarily
- Refrain from asking multiple questions in succession
- Pause frequently, allowing up to 20 seconds of silence for processing after asking questions or giving directions
Meet Urgent Needs: Address immediate concerns and basic needs before moving to complex medical discussions. This might include pain management, comfort measures, or simply acknowledging their distress.
Avoiding Communication Pitfalls
Certain phrases and behaviors can inadvertently trigger trauma responses. Vistelar identifies several "trigger phrases" that healthcare professionals should avoid:
- "Calm down" or "Relax"
- "What's your problem?"
- "You wouldn't understand."
- "Those are the rules."
- "You always/never..."
- "You're overreacting."
- "That's not my job"
- “You need to…”
- “No one is going to hurt you…”
These phrases, while sometimes said with good intentions, can activate a patient's trauma responses and escalate rather than de-escalate difficult situations.
Use Safety Statements
Avoid reassurances like, “This won't hurt,” or “No one is going to hurt you.” Or warnings like, “This will hurt just for a second.” The “hurt” word is a common mistake when working with patients. Instead, use safety statements, phrases and synonyms:
- “You're safe now.”
- “We will take care of you.”
- “This will make it feel better.”
- “This will only pinch for a moment.”
Patients experiencing or remembering pain, fear, or trauma will sometimes only hear the word “hurt,” especially if they are children, trauma survivors, or living with cognitive impairments or mental illness.
Victims of sexual and other abuse were also often told by their attackers, “I won't hurt you,” or “This won’t hurt.” This common pitfall–the “hurt” word–can lead to severe re-traumatization of abuse survivors.
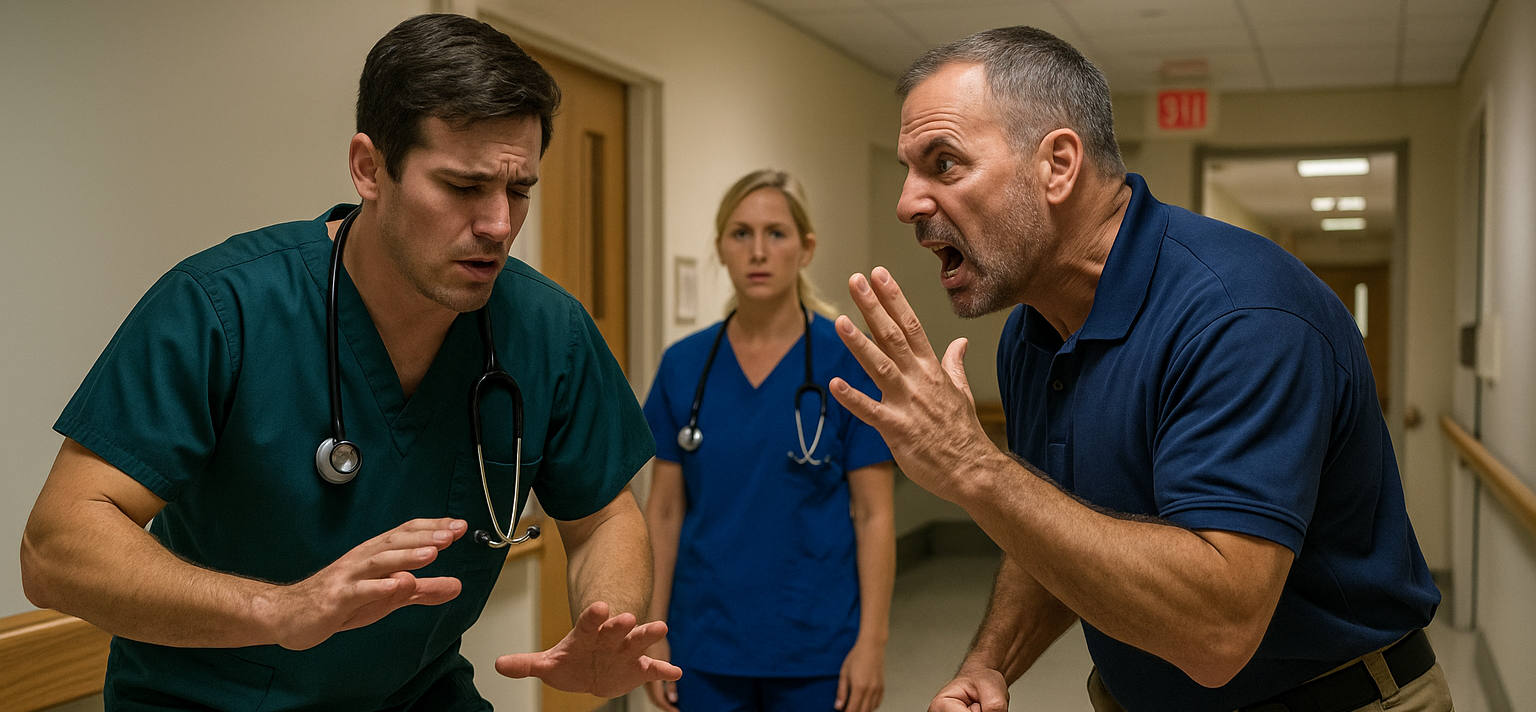
Maintaining Your Emotional Equilibrium
Healthcare professionals working with trauma survivors must also protect their own emotional well-being. Vistelar's "Respond, Don't React" principle becomes particularly crucial in these interactions.
Identifying Your Conflict Triggers
Self-awareness is the foundation of effective trauma-informed communication. Healthcare providers should regularly examine their own past experiences and identify personal conflict triggers that might interfere with patient care. Common triggers in healthcare settings might include:
- Patients who remind you of personal experiences
- Specific types of trauma histories
- Aggressive or demanding behaviors
- Situations that challenge your professional competence
Maintaining Professional Presence
The Showtime Mindset ensures that healthcare providers remain emotionally, mentally, and physically prepared for challenging interactions. This means:
- Aligning your proxemics (body position), verbals (words), non-verbals (body language), and paraverbals (tone of voice)
- Avoiding misaligned communication, such as smiling during serious situations
- Remaining alert and decisive while maintaining a calm, professional demeanor
Applied Proxemics: Managing Space and Safety
Understanding how to manage physical space becomes particularly important when working with trauma survivors. Vistelar's Applied Proxemics provide specific guidelines:
The 10-5-2 Approach:
- 10 Feet: Evaluate and assess—at this distance, you can observe and decide whether to approach or maintain distance
- 5 Feet: Normal social interaction distance for most healthcare conversations
- 2 Feet: Close interaction distance, used only when necessary and with clear consent
Tactical Positioning: When sitting with patients, use tactical sitting techniques—sit at the corner of your seat with your non-dominant foot centered and dominant foot positioned for mobility. Keep your hands visible and be prepared to move if the situation changes.
Beyond Active Listening: Gathering In-Depth Information
For patients with trauma histories, standard active listening may be insufficient. Vistelar's "Beyond Active Listening" technique provides seven elements for deeper engagement:
- Clarify: Ask open-ended, opinion-seeking questions
- Paraphrase: Reflect back what you understand in your own words
- Validate: Acknowledge their feelings without necessarily agreeing with their perspective
- Empathize: Show that you understand their emotional experience
- Inquire: Ask follow-up questions to deepen understanding
- Paraphrase Again: Confirm your understanding has evolved
- Summarize: Bring together the key points of your conversation
This approach helps patients feel genuinely heard and understood while providing healthcare providers with the information needed to deliver appropriate care.
Implementing Trauma-Informed Communication Organization-Wide
Healthcare organizations that implement comprehensive trauma-informed communication approaches consistently see:
- Improved Patient Engagement: Patients feel safer and more willing to participate in their care
- Enhanced Treatment Adherence: When patients trust their providers, they're more likely to follow treatment recommendations
- Better Health Outcomes: Addressing trauma's impact on health leads to more effective treatment
- Increased Patient Satisfaction: Respectful, understanding care creates positive healthcare experiences
- Reduced Risk of Re-traumatization: Thoughtful approaches prevent healthcare encounters from becoming additional sources of trauma
Moving Forward: A Call to Action
Trauma-informed communication represents more than a set of techniques—it embodies a fundamental shift in how we approach human interaction in healthcare settings. By integrating Vistelar's evidence-based conflict management principles with contemporary understanding of trauma's impact, healthcare professionals can create environments where healing truly becomes possible.
Every healthcare encounter is an opportunity to demonstrate dignity, respect, and genuine care. For patients carrying the invisible wounds of trauma, these interactions can become turning points—moments when the healthcare system shifts from being a source of additional stress to becoming a place of genuine healing and hope.
The question isn't whether your patients have experienced trauma—statistics tell us they almost certainly have. The question is whether your organization is prepared to recognize, understand, and respond to trauma in ways that honor each person's dignity and support their journey toward healing.
As healthcare leaders and professionals, we have both the opportunity and the responsibility to transform our communication practices. By embracing trauma-informed approaches rooted in empathy, respect, and genuine understanding, we can ensure that every patient interaction moves us closer to the healing-centered care that defines healthcare at its best.
This blog post integrates Vistelar's evidence-based conflict management principles with current research on trauma-informed care. For comprehensive training in these techniques, explore Vistelar's healthcare-specific conflict management programs designed to enhance both patient care and staff safety.