In healthcare settings, first impressions aren't just about customer service—they're critical safety moments that set the tone for everything that follows. Those initial 10 seconds of contact between a healthcare provider and a patient or visitor can determine whether an interaction proceeds smoothly or escalates into conflict.
As we observe National Safety Month this June, it's worth examining how these brief but crucial moments impact safety throughout healthcare organizations. Many workplace conflicts, security incidents, and even clinical misunderstandings can be traced back to how an interaction begins.
The Science Behind First Impressions
Research consistently shows that humans form initial impressions with remarkable speed:
- Princeton University researchers found that people make judgments about trustworthiness, competence, and aggression within the first 100 milliseconds of seeing someone
- Communication studies reveal that tone of voice, facial expression, and body language account for over 90% of first impression formation
- Neurological research demonstrates that these snap judgments trigger emotional responses that can be difficult to reverse once established
In healthcare settings, where stress and anxiety are already elevated, these rapid assessments take on even greater significance. A patient or family member who feels dismissed, rushed, or disrespected in those first moments may remain on guard throughout their entire encounter.
The Safety Impact of Initial Contact
The way we begin interactions doesn't just affect customer satisfaction—it has tangible safety implications:
For Patient Safety:
- Patients who feel respected and heard in initial contact are more likely to disclose critical health information
- Trust established in the first moments increases medication and treatment adherence
- Clear, respectful communication from the start reduces miscommunication that can lead to errors
For Staff Safety:
- Professional initial contact reduces the likelihood of verbal and physical aggression
- Proper greeting and introduction establishes authority and boundaries
- Structured openings demonstrate attention, concern, and psychological safety for apprehensive or fearful patients and clients, thereby increasing staff safety
For Organizational Safety:
- Consistent professional openings reduce complaint rates and liability exposure
- Standardized greetings ensure critical information isn't missed
- Professional first impressions build trust that can buffer against later difficulties
The Universal Greeting Framework
At Vistelar, we teach the Universal Greeting as a foundational skill for establishing safety in the first moments of contact. This structured approach includes four key elements:
1. Appropriate greeting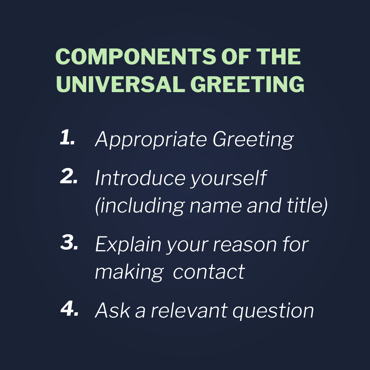
Begin with a time-appropriate greeting ("Good morning," "Hello") that acknowledges the other person as a person worthy of respect.
- Crowding or invading personal space
- Blocking movement or access
- Aggressive positioning or combative stance
2. Name and affiliation
Identify yourself and your role clearly ("My name is Sarah, and I'm one of the nurses who will be caring for you today").
3. Reason for contact
Explain why you're initiating the interaction ("I'm here to take your vital signs and ask a few questions about how you're feeling").
4. Relevant question
Invite participation with an open-ended question that gives the other person a voice ("How has your morning been so far?").
This framework accomplishes several safety objectives simultaneously:
- It establishes your professional identity and authority
- It gives the other person context for the interaction
- It demonstrates respect by inviting participation
- It creates structure that reduces uncertainty
Beyond Words: The Full Spectrum of Initial Contact
While the Universal Greeting provides a verbal framework, the first 10 seconds of safety involve multiple dimensions:
Physical Positioning
The Proxemics 10-5-2 rule guides safe positioning:
- At 10 feet: Evaluate the situation and decide whether to approach
- At 5 feet: Begin verbal communication while maintaining a safe distance
- At 2 feet: Only enter this intimate space when necessary and safe
This structured approach to physical positioning prevents the common mistake of getting too close too quickly, which can trigger defensive reactions in anxious or agitated individuals.
Non-verbal Elements
Critical non-verbal aspects of initial contact include:
- Appropriate facial expression matching the situation (not smiling during serious discussions)
- Open body language that appears non-threatening
- Eye contact that shows attention without staring
- Hands visible and empty to demonstrate lack of threat
Paraverbal Components
How we speak carries as much safety significance as what we say:
- Calm, measured tone regardless of the situation's intensity
- Volume appropriate to the setting (not too loud or too soft)
- Pace that allows for comprehension (slower than normal conversation)
- Pitch that conveys confidence without aggression
Training for the First 10 Seconds
Developing proficiency in safe initial contact requires dedicated training:
1. Scenario-based practice
Role-play various first contact scenarios:
- Greeting anxious family members
- Approaching agitated patients
- Initiating difficult conversations
- Responding to hostile initial contact
2. Video analysis
Record and review initial contact moments to identify:
- Unconscious behaviors that might escalate tension
- Misalignment between verbal and non-verbal messages
- Opportunities to enhance professionalism and safety
3. Standardized frameworks
Develop and implement standardized greeting protocols for:
- Different departments and roles
- Various patient populations
- Common high-risk situations
- Phone and in-person interactions
4. Feedback mechanisms
Create systems for monitoring and improving initial contact:
- Peer observation programs
- Patient/visitor feedback specific to first impressions
- Incident analysis that includes assessment of initial contact
- Regular refresher training on greeting protocols
Implementing First-10-Seconds Safety
To maximize the safety impact of initial contact, consider these organizational strategies:
Leadership Modeling
Leaders should exemplify proper greeting protocols in all interactions. When executives and managers consistently use the Universal Greeting, it signals its importance throughout the organization.
Environmental Support
Create environments that support effective initial contact:
- Adequate time for proper greetings (not overwhelming staff with patient loads)
- Physical spaces that allow for proper distancing
- Visual reminders of greeting protocols in staff areas
- Reduced distractions at points of first contact
Cultural Integration
Embed initial contact awareness into organizational culture:
- Include greeting protocols in onboarding and orientation
- Recognize and reward exemplary initial contact behaviors
- Share success stories of difficult situations managed through effective first contact
- Incorporate initial contact quality into performance reviews
The Compounding Benefits
Investing in those first 10 seconds creates compound safety benefits throughout the healthcare journey:
- Trust established initially makes later difficult conversations easier
- Professional distance created at first contact provides buffer during stressful moments
- Information gathered through effective openings improves clinical decision-making
- Respect demonstrated from the start reduces complaints and improves satisfaction
This National Safety Month, consider how your organization might enhance safety by focusing on those critical first moments of contact. By treating the beginning of every interaction as a safety event—not just a service opportunity—we create foundations for safer healthcare environments for everyone.