There is no denying it; hospitals can be difficult places to work. No matter which profession you’re in, from hospital security to nursing, the hours are long, and weekends and holidays are just another day at work. Moreover, with nursing shortages, an aging demographic, dwindling psychiatric care resources, and other factors creating increasing demands on healthcare providers from all sides, the healthcare profession around the world is entering into its most challenging phase of the postmodern era.
The good thing is that we’ve finally stopped hiding the fact that healthcare—as far as violence is concerned—is one of the most dangerous professions in America. In my own career, I’ve been in scores of physical altercations. Providers have become so accustomed to violence that they think of it as just being part of the job. However, we must stop thinking that way because, as in any relationship, the behavior we accept is the behavior we support.
Visiting Hours Are Over
On one particular evening, I was repeatedly sent to an in-patient unit for noise complaints involving the same patient and her family. It was after 10:00 PM, and visiting hours were officially over at 8:00 PM. This was my third trip back to the unit. I didn’t escort the family off the unit after the first complaint around 8:30 PM because the term “visiting hours” was just treated as a suggestion at this hospital. In fact, many hospitals in the region even practiced 24-hour open visitation in those days. They referred to this as a facet of patient-centered care. Today many hospitals have abandoned open visitation as a general practice due to the problems it creates.
Needless to say, I wasn’t very enthusiastic about going back to that unit. All the nursing staff expected me to do was ask them to be quiet. It was a frustrating cycle that we had gotten into at the hospital, and as a result, the number of noise complaints were affecting patient satisfaction scores. In fact, in the profession, noise is the number one complaint that in-patients report in their patient satisfaction surveys. When I arrived at the unit, I went to the charge nurse to get briefed before returning to the patient’s room.
“I didn’t call you,” she said.
“But the dispatcher said someone called again about the noise in room 702,” I replied.
Looking surprised, she asked the patient’s nurse and other staff who might have called. Finally, a nursing assistant spoke up and said, “The guy in 703 called and he’s mad.”
After responding back to room 702 and finally convincing the family members to leave, I went to room 703 to talk to the patient who had called in the complaint. After introductions, I filled him in that the patient’s visitors had finally left.
After a deep sigh, he asked, “Why did you let them stay up here so late?”
“Well, we tend to bend the rules for people sometimes; we try to respect people’s needs.”
“What about my needs? I’m trying to recover from surgery. I’ve been trying to sleep for two hours and I’m in pain!”
Looking at the Problem From the Wrong Angle
With that response, the light finally came on for me. We had been looking at the problem with patient satisfaction from the wrong angle at this hospital. In fact, with a little research, I discovered the healthcare.png?width=225&name=Blog-GraphicArtboard%201%20(2).png) profession across the whole country had been looking at it from the wrong angle. By focusing on the individual wants and demands of some, we were trampling on the rights and needs of others. Before long, I decided to go on a campaign to change things.
profession across the whole country had been looking at it from the wrong angle. By focusing on the individual wants and demands of some, we were trampling on the rights and needs of others. Before long, I decided to go on a campaign to change things.
The first step was to talk to my supervisor and my director. I explained to them that when we focus so much on the demands of an individual patient, we forget about all the other patients around them. I also suggested that we needed to start enforcing visiting hours and limits on cursing, yelling, threatening, and even rude behavior. For this to be successful, I told them we needed the nursing staff and doctors to get on board and raise the expectation of behavior for all.
They admitted that everything I was saying was correct, but they were not ready to abandon the point of view of the hospital administration that the customer is always right. They also knew that starting to enforce the little rules would likely generate more complaints. I was disheartened by their response, but soon their minds would change entirely.
Gateway Behaviors and Healthcare Violence
With my director’s support and encouragement, I talked to everyone who would listen. I made appointments with risk managers, patient relations people, hospital administrators, physicians, behavioral health providers, and nursing administrators. Soon with a lot of convincing and ultimately their help, I developed my elevator speech: “Gateway Behaviors and Healthcare Violence.” The concept was simple.
First, if you allow someone to disrespect you verbally (yell, curse, call you names, and refuse to follow simple rules) they will feel emboldened. That’s because if someone is verbally disrespecting you, it’s like sending out radar waves to see what bounces back. If what bounces back at them is silence, the nonverbal messages are: a) it’s okay to behave that way; b) this person has no authority to do anything about it; and, c) this person is afraid to do anything about it.
All in all, there are no positive messages if you are silent when disrespected or threatened.
In fact, once someone feels comfortable disrespecting you, they often start to threaten you. It usually starts out in the form of a veiled or implied threat, such as, “I’ll have your job!” or “Come in here again and see what happens.” Then if we say nothing, they sometimes flat out start threatening you, “Touch me again and I’ll jab that needle in your face!” I’ve worked, consulted, and trained in lots of different professional spaces, but healthcare is the only profession I know of where you seem to be able to threaten people with impunity. It’s time to ask ourselves if that level of tolerance keeps us safer.
The answer is simple. Even though the victims of violence often say, “the attack came out of the blue!” it rarely ever does. Typically, people tell us many times they are going to hit us before they do it. Sometimes they do it with their facial expression or other visual threat indicators. Sometimes they say it with their tone and volume. Sometimes they warn us by threatening us verbally. Tragically, we help them make the decision to strike with our silence, inaction, and even appeasement.
For many of us, it’s natural to fight fire with fire. The trouble with that is we just end up burning our own house down. They yell, so we yell back. They threaten, and we threaten back. This isn’t the right approach of course, but for the inexperienced and untrained, it’s what they know. For others, it’s natural to submit to the common response of killing them with kindness. But does that really work? If someone told you their significant other was verbally abusing them, would you tell them to kill them with kindness? Of course not. So why do we keep giving each other the same terrible advice in healthcare?
Inherently, violent relationships develop the same way—whether they are domestic or professional. The behavior you allow is the behavior you’ll get. And if you don’t stop the cycle at the low-end (disrespect) it will escalate to the high-end (physical violence).
How do we stop this?
First, we have to say enough is enough. Then we have to remind ourselves that most people treat us with respect. It’s only the few that treat us badly that we have to learn to manage better. Then we must set the example: we need to treat each other with dignity by showing each other respect.
Frankly, those of us in healthcare have a reputation for unhealthy professional relationships. Why is that? Again, it’s simple. The old guard of nursing has a saying, “Nurses eat their young.” Nursing has a reputation for high levels of interprofessional passive-aggressive behavior. In fact, studies have indicated that there is an acute problem with professional relationships in healthcare. If you work in a high-stakes profession that is known for conflict with many of its customers, it is easy to see how that could affect your professional relationships as well.
Finally, we must start setting limits on the gateway behaviors of violence exhibited by a small number of healthcare consumers that behave badly. No one wants to be in the hospital; many people show up in pain, sick, scared, under-insured, and with all the resulting financial, personal, and professional problems that health problems generate. However, that doesn’t mean that we can’t set expectations for mutual respect.
It’s time for those of us in the healthcare profession to ask ourselves some questions. Do you know what the expectation for behavior is at a library and are those expectations enforced? Do you know how to behave when in a place of worship? How about a movie theater? Maybe even a bank? But the real fundamental question is this: What is the expectation for behavior in a hospital?
Once a healthcare system decides to turn things around, it’s not enough just to tell staff to stop letting people behave disrespectfully. That’s just a path to more conflict. What you need to do is train them on when and how to do this, and on the difference between antisocial gateway behavior and crisis behavior. Both are common problems in healthcare and need to be addressed in different ways. The facts are that untrained providers aren’t good at managing either.
A Simple Tactic
Here’s a simple method we implemented at the hospital after we were properly trained.
“Hello Sir, I’m Joel from Security. I hear that you are upset and I’m going to do whatever I can do to help. But can I ask you not to yell and curse? There are patients and children around. Some of them might have heart conditions and the kids might be scared hearing you yell. This has to be a safe and appropriate environment for everyone. Now, tell me what’s got you so upset today.”
That simple approach has the power to reset and redirect-gateway behaviors. Along with that skill set, people needed to be trained in distance and positioning to keep safe. They also needed to know what to say and do if it didn’t work along with many other methods that enable healthcare providers to set limits and recover clinical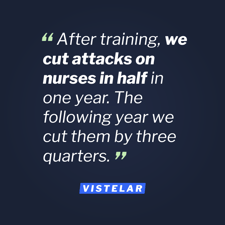 relationships. After training, we cut attacks on nurses in half in one year. The following year we cut them by three quarters. Soon, hospitals around the country were asking how we did it.
relationships. After training, we cut attacks on nurses in half in one year. The following year we cut them by three quarters. Soon, hospitals around the country were asking how we did it.
I spent the next couple of years writing books and articles, and touring and lecturing on the concepts of gateway behaviors and social contracts in medicine. There are two proud moments that stick out for me when reflecting on my success of this.
One was when a security officer told me that he was walking through the emergency room waiting area at the hospital where I used to work when he heard a man cursing and yelling on his cell phone. Then, the officer saw a woman nudge him and say, “They don’t play that here.” At that, the man stopped yelling and cursing.
The other was when a hospital security department called a hospital where we had trained staff extensively and asked, “We had a loud scene in the ED waiting room the other day and a woman complained about it. She said they would never allow that at your hospital. What are you guys doing over there?”