“Trauma Informed Care and Why It Matters ” - Episode 7
Host: Al Oeschlaeger
Guest: Debbie Zwicky
Subscribe to our podcast on Apple Podcasts, Stitcher, Google Play or YouTube.
People living in treatment centers have often experienced multiple traumatic events in their lives. Adolescents and young people are a particularly vulnerable group in these facilities. Trauma Informed Care is an important component to keeping residents and employees cared for and safe. Debbie Zwicky worked for 27 years as a youth care worker and shares how practicing empathy, “seeing the world through their eyes,” assisted her in keeping adolescents in her treatment facility safe.
Allen: Well good morning Debbie.
Debbie: Good morning.
Allen: Good to talk to you again. Debbie, as I mentioned, is one of our trainers, so I see her in the office all the time. So we’re going to be talking about your background today, which is rich with conflict. Tell me, how did you get into youth care? Is that what you call it?
Youth Treatment Centers
Debbie: Yes. I started out as a youth care worker. It was kind of by accident actually, which as I found as I worked in youth care work, happens a lot of times to people. It’s not a traditional path like some careers or positions are. But I did an internship at the Boys and Girls Club in Indiana when I was in college, and I’ve found I really enjoyed working with young people, adolescents, so I came back home to Wisconsin and started my job search here. And actually at the time, my mom was a nurse at the blood center, and she happened to have somebody come in and give blood and they were chatting and it happened to be a therapist at a treatment center in the city. And she said “Oh, my daughter’s looking for a job,” And he said “Oh, have her come apply,” And I did, and that’s how I got started in youth care work.
Allen: Wow. So tell me … The treatment center, I think a lot of people don’t know that term, so what’s that mean? Treatment center.
Debbie: Treatment center is basically a facility for … The one that I worked in was for adolescents, so we had young people ages 8 to 18, and they were there court ordered into treatment. And they were there for a variety of challenges, issues, things that they were dealing with. We saw a lot of history of trauma, abuse, neglect, family issues, family disfunction, a lot of school issues, a lot of behavior issues. Especially for the young ladies who were between the ages of 8 and 12, that’s pretty much how they were dealing with a lot of their trauma, was acting it out in their behavior and therefore they were really having troubles at home and in school. And that is the reason that they were coming to our treatment center, to have group therapy, individual therapy, milieu therapy, and the youth care workers were the direct care workers that were working on the units 24/7.
Allen: Court ordered. Court ordered because why? Is that because of a parent situation? How do you get to court ordered treatment?
Debbie: It could be either. Typically there were two types of court orders, either they were coming in through a delinquency court order, so they had had some issues with law enforcement, or they were coming in through what is called a CHIPS order, which is a child in need of protective services and they needed treatment for that reason or they needed to be removed from the home. Which usually also entailed them needing some treatment. So they would come into our treatment facility and we would also do family therapy, and the goal was to reunite them at home. Or in a foster home.
Allen: And is there treatment centers that are not court ordered that are somehow different?
Debbie: It kind of depends. For youth they’re court ordered, not so much always for adults.
Allen: So what would that be called, if you had a facility where adults came and it wasn’t court ordered? What would you call that?
Debbie: You may call it a health center, or they may just be going for outpatient services where they don’t live there but they’re just getting outpatient treatment and they’re living at home independently.
Allen: Wow. I should know this Debbie, but how long were you doing this before you came to work with us?
Debbie: 27 years.
Allen: 27 years.
Debbie: Right out of college.
Allen: And at any given time in this treatment center, how many … What would you call it, clients?
Debbie: We called them residents.
Allen: Residents, okay. How many residents would there be?
Debbie: Our maximum bed capacity was 40.
Allen: Okay. And they live there, so they slept there and it was-
Debbie: They lived there. We were open 24/7, staffed 24/7, we had four units that could hold up to 10 young ladies at a time.
Allen: And did they have home visit rights?
Debbie: Yes.
Allen: Oh yeah, okay.
Debbie: [crosstalk 00:04:53] they could have visits at the place, sometimes families came to visit and we had visiting rooms and places that they could go, or they could go outside or they may leave for a couple hours and come back and then they could work up to a full day at home, overnights at home, weekends at home, holiday breaks at home. And that would be written into their treatment plan as far as their goal to go home.
Allen: Okay. And at any given time, everybody had some of that going on? Or some were really-
Debbie: Unfortunately we had some young ladies who never had home visits while they were in our program.
Allen: And they stuck around for how long? How long were they there?
Debbie: Average placement, depending on the time, six months was probably fairly average. So some were maybe there two to three, some were there maybe eight to nine. Once in a while we had girls there about a year, but that was pretty rare.
Allen: As you know Debbie, the class we did … Whenever it was, what, a week and a half ago? And we started out and I asked the question, “How many people have seen any conflict in their life?” Right? And everybody’s hand went up immediately. So obviously your hand would have gone up.
Debbie: Absolutely, absolutely.
Allen: [inaudible 00:06:15] So describe, for the listeners, just a little bit about what you end up dealing with. Because I don’t think people have too much awareness of what happens in a treatment center.
Debbie: Well, like I mentioned, we were dealing with for the most part adolescent young ladies. We did, for a short time, have programs where we had adolescent males in the facility in a group home facility. So a lot of the conflict was them A, trying to figure out how to all live together, if you can imagine 10 adolescent girls living in a space, and 4 of those spaces in a building. Some of it obviously was just how to manage day to day functioning, and they were also dealing with some deficits and some challenges. So they didn’t have a lot of good skills in that area of conflict management and empathy and treating people with dignity by showing respect. So we worked on a lot of those every day, individually, in groups, of just those concepts and how to deal with anger.
Debbie: I saw a lot of angry young people. And with good reason as you looked at their history and their trauma and their family situations. So we worked a lot with how to kind of manage that day to day, how to manage frustration, how to manage disappointment, how to identify and manage your feelings about those things as they worked through some of their trauma and history and those types of things. And when you have numerous young ladies doing that at the same time, there was definitely a lot of conflict.
Allen: And I’m assuming nobody got a private room, is that a fair assumption?
Debbie: The only time that would happen is if we weren’t full, if they didn’t have 10 on a unit, then sometimes they would have their own room.
Allen: But otherwise it was two people a room, or more?
Debbie: Correct. We had a couple single rooms just if their treatment plan dictated that, so I will take that back. We did have a couple single rooms and some double rooms, because sometimes their treatment needs dictated that they needed their own room. For safety reasons.
Trauma Informed Care
Allen: [crosstalk 00:08:41] so you mentioned trauma, and I know that … I don’t know exactly the time frame, a couple years ago, you got involved in a different thing. You left the treatment center and you got involved as being a trauma something something coach.
Debbie: Correct, I was coaching teams throughout the state of Wisconsin on trauma informed care. And that was a little bit different perspective or different spin on it, because we were really looking at the staff and the workers and how they deal with trauma within their agencies and within their staff. Versus how you deal with it with clients or residents. Because research shows that just in the regular population there is a high percentage of people who are dealing with trauma.
Allen: Yeah. Like everybody [crosstalk 00:09:32]
Debbie: So we’re looking at it kind of from a different perspective of your staff and your coworkers, and how you would manage that within the workplace, especially if part of your job was to have clients who also had trauma. So how that was all interwoven and how you dealt with that internally well, so that you could then deal with it well with your clients and residents.
Allen: What would be an example of clients? What kind of clients were you dealing with? Other residential treatment centers, or …
Debbie: Yes. Some of them were case workers, some of them were public defenders, some of them were other social service providers that were dealing with clients in the community.
Allen: I got it. So in this trauma informed care, as you know, we’ve … What, it’s been probably five years that we’ve incorporated into our curriculum on how to deal with conflict. But it’s been around for a long time, right? Its origins go way back, I think? Right? The history?
CDC-Kaiser Study on Adverse Childhood Experiences
Debbie: Yes. I think it really started when they did what was called an ACE study, and that was done through the Center for Disease Control, along with Kaiser Permanente, which was an insurance company. And they really were looking at what they ended up calling adverse childhood experiences, which is basically childhood trauma. And they were wanting to see-
Allen: So that’s the ACE, the acronym ACE, it means adverse childhood … What is it? Experiences?
Debbie: Experiences, uh-huh (affirmative).
Allen: Okay.
Debbie: So they were looking at those things that were creating trauma for children in their lives and in their families, and they wanted to look at how that impacted health issues as an adult. Things such as diabetes, obesity, things that insurance companies pay a lot of money for to help people heal. And they found a lot of links to that, and they found that those ACEs, as they’re called, definitely were affecting adult health. If you had … Over four seem to be kind of the mark when they really started to see, and there’s ten total, high percentages of adult health concerns in those people.
Allen: What was the time frame for that? Do you have any number [crosstalk 00:12:10]
Debbie: That happened between 1995 and 1997, about was when that study and those people were involved in that through Kaiser Permanente.
Allen: So given you were involved in residential treatment, would you have known about that back then, or was that well known?
Debbie: Yes, yes. The state of Wisconsin became very involved in that.
Allen: Right away.
Debbie: Yeah, right towards the end of the 90’s. And there was a lot of focus in the state, especially within the residential treatment centers, behavior health, of utilizing the ACE assessment tool and really looking at childhood trauma and making that a focus for their treatment planning.
Allen: So its origins were primarily in social work then? Or in healthcare, or in schools? Do you know where it got most of its initial …
Debbie: I think it was healthcare and social services, and then I think it really moved into the school systems after that.
Allen: Okay. So give some examples of what an ACE is. What would be a … You said there’s 10 of them.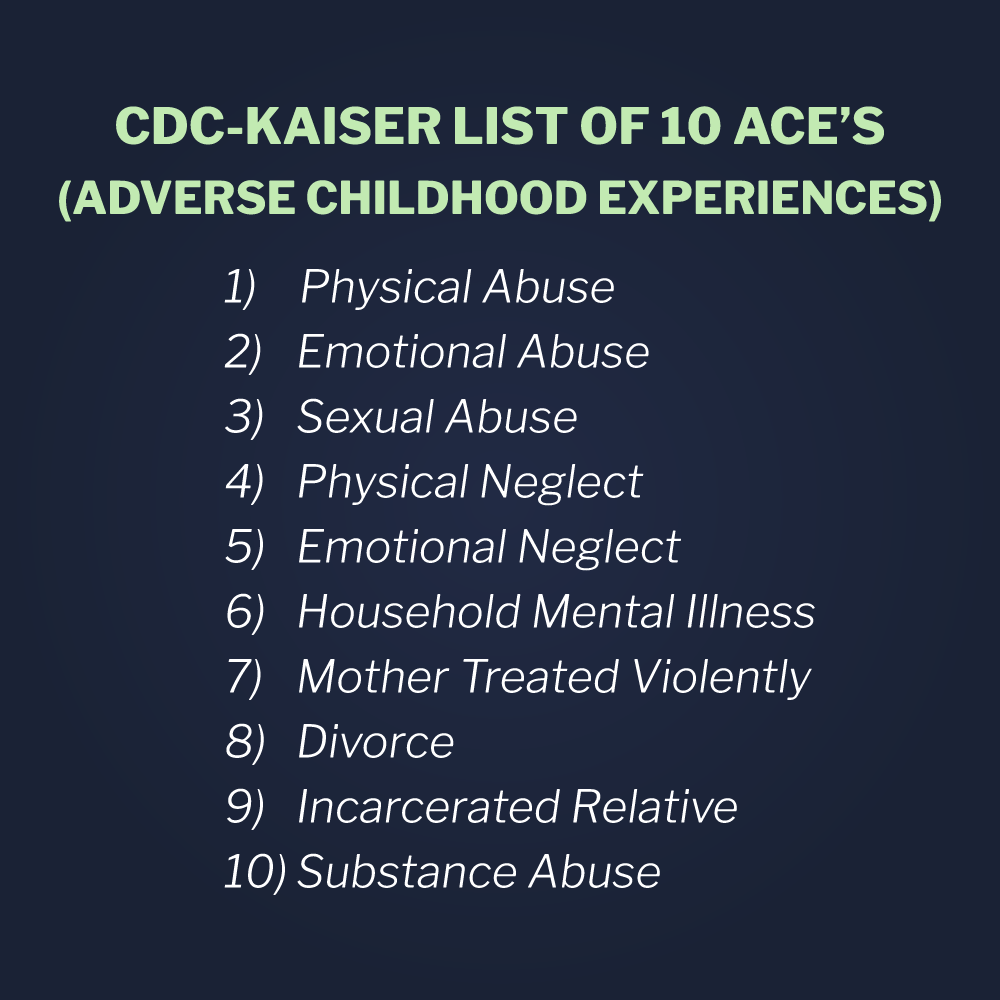
Debbie: Yeah, yeah. It’s an assessment questionnaire, and you score yes or no if you’ve had any of those within your childhood. And those childhood adverse experiences could be things like incarceration, were there any people in your home that were incarcerated? They look at drugs and alcohol, they look at divorce, they look at abuse, they look at neglect. So those are the things they’re targeting.
Allen: So it’s a pretty simple questionnaire, you either had that experience or not.
Debbie: Correct. [crosstalk 00:14:07] basically check yes or no.
Allen: Yep, across these 10, and if you have more than 4, then there’s pretty strong evidence that that leads to adult health problems.
Debbie: Correct. And there’s even evidence that one to two does, but it really seemed like that four really spiked some results there. And then obviously the more you have … And I would say in places like psychiatric hospitals, treatment centers, AODA treatment centers, it’s probably higher. The average I would say in our treatment center was probably eight.
Allen: Oh, wow. Oh, wow.
Debbie: Most of our residents scored fairly high.
Allen: And then it’s my understanding that Wisconsin … You already said we got involved in the late 90’s, but we’ve been kind of a leader on this in terms of other places.
Debbie: [crosstalk 00:15:08] Yes, yes, yes. And there’s been a lot of funding and efforts and focus groups and things that have happened within the state of Wisconsin and are still happening, to deal with the childhood trauma issue here in the state of Wisconsin.
Allen: I think it was about a year ago Debbie, maybe a little longer, that there was a … I think there was some state grant money to schools that was maybe focused on safety. I think it was maybe post one of the school shootings.
Debbie: Absolutely.
Allen: [crosstalk 00:15:42] But if I remember [inaudible 00:15:43] they couldn’t get their grant money unless some high percentage of the staff had been through a trauma informed care program.
Debbie: Correct. And they’re finding …
Allen: I think [crosstalk 00:15:54][inaudible 00:15:54]
Debbie: And they’re finding a lot of connection, obviously, between safety and trauma informed care and ACEs and those types of things, because trauma and safety are definitely intertwined. And kids and people who have been through trauma really have some challenges coping to feel safe within their day to day life. And obviously children spend a lot of time in school, so it made sense to get the school community onboard. And they typically use a term called trauma sensitive schools, whereas they’re really working into their curriculum and their day to day plan with the kids in their schools to be trauma sensitive.
Allen: Yep. And I know within this [inaudible 00:16:48] we’ve kind of started using the term trauma responsive, I’m not sure exactly where that came from, but that’s our term because we generally are dealing with conflict in a real time situation and it’s making sure that our actions are responsive to the other person’s past trauma. I think there’s a reason for trauma responsive. It started as trauma informed care, with trauma informed meaning that your care should be based on being informed of the other person’s trauma, if I understand it right. Do I? Is that the right interpretation of trauma?
Debbie: Yes, I think that was the first term, and then obviously as more research was being done and people started to utilize the ACE study and work with people who have had trauma in their life and are currently healing from that trauma, other things develop from that. And I think that’s where some of the other terms started to come from. And like you said, depending on your role within that and what you were utilizing or looking at or paying attention to within trauma. And that’s, I think, how some of the other offshoots of terms came to be.
Allen: Obviously a school, they do care for their students, obviously, but they don’t use that term. As you know, we deal with a fair number of education clients in the state and they all use the term, and I think it comes from the department of instruction, trauma sensitive schools is the term used there, and then trauma informed care is used I think in social services and in healthcare. And then we talk about trauma responsive conflict management, because that’s our focus. So, interesting. Do you have any idea what … I know that at the administrative level within the state there was a fair amount of emphasis, but why did Wisconsin become a leader? What drove that, compared to other states? Why are we ahead of the curve and been doing this for so long?
Debbie: I think one of it was it was just kind of a passion within the governor’s office at the time, and the governor’s wife got very involved with it and really felt that it was something that could help Wisconsin. There’s a lot of trauma in the larger cities in Wisconsin, you look at Milwaukee, Madison, where there’s a lot of families struggling, and a lot of that struggle stems from the trauma that’s being created. And then you also have the trauma in the more rural counties that’s focusing around the meth and the opioids and the drug use, and you find a lot of trauma obviously interwoven into the drug addictions and those types of things. So I think there was a lot going on here in this state, and it was a way hopefully to help us wrap our minds around that and to help those people heal.
Allen: And from what I understand, there really isn’t any controversy about this anymore, right? I’m sure when the study first came out people questioned the results, but after all these years now I think this is pretty well set, that if you have childhood trauma and it’s at some meaningful level, you’re going to end up with some kind of issues later in your life.
Debbie: There’s definitely your risk gets a lot higher. And some of it makes sense. You look at obesity for instance, food is a coping skill for a lot of people, and a lot of people who struggle with obesity use it for that. So the two kind of make sense, that if you’re dealing with a lot of trauma and you’re dealing with a lot of abuse and neglect and drug and alcohol issues and family issues and school issues and behavior issues and food is your coping skill, you’re probably going to be eating a lot because you’re going to be in a lot of unsafe situations. So some of it, you can see where the correlation would be there. And obviously as time goes on you get more data and you get a little bit better at it. So hopefully at some point we’ll see those going down, because we’ll really get a better understanding of how to help those people heal and how to help those families heal.
Trauma Informed Care In Action
Allen: So I know you have a little story that illustrates … I’m not sure where it’s from exactly, so I want you to introduce the story and then I think it just illustrates what we’ve been talking about here.
Debbie: Yeah. Like I said, working in a residential treatment facility we had a lot of times where kids really struggled with behavior that was kind of driven by their trauma. And a lot of times we saw it when their parents would come visit, especially if their relationship with their mom, we saw a lot of moms with their daughters and how important that relationship is and how fragile that relationship can be and how tough that relationship can be, especially if mom also dealt with some trauma. If her ACEs are pretty high, if the daughter’s ACEs are pretty high, sometimes their interactions can be pretty conflictual. And I saw that firsthand one time when I was walking through the front lobby and we had a young lady who was visiting out in the community with her mom for the first time in a long time, and there was a long history of a lot of challenges between those two and a lot of physical fights and those types of things and that’s how they just knew to communicate. And we were working with them on how to do that better.
Debbie: So we were all informed that she was on this visit with her mom and that she was on her way back, and I happened to be walking through the front lobby and saw them in their car in front as mom was dropping her off. And I could tell by the body language within the car that they were having a pretty heated discussion. And knowing their history, I thought “You know what, let me just see where this goes.” So I kind of hung out there for a while and it got a little more heated, and the young lady opened the door on her side to get out and I could then hear that it was pretty loud, and some pretty abusive language was happening, and I realized that this situation wasn’t going well and their interaction wasn’t very healthy at that time. And I knew they had some history of becoming physical, and definitely we didn’t want that to happen for their safety. So I phoned some help, we got some staff out there, we actually ended up having to physically intervene between the mom and the young lady, and I was pretty used to, unfortunately, physically intervening with young people, but not so much a mom or an adult.
Debbie: So that was a little bit of a different experience, and I really had to remind myself of where she was, and put myself in her shoes, being a mom at that time, that was something that was kind of out of my wheelhouse as far as how she was interacting with her daughter. But I had to remind myself that she was in a different place and her history was very different than mine, and I had to really see the world through her eyes at that time and what was going on. And I had to remember my proxemics to keep myself safe, so there was a lot going on.
Allen: Let me jump in here. One word that I’m sure nobody hears or understands, because I didn’t know about it until several years ago, but first question. When did you first get involved in the [inaudible 00:24:53] training material? How long ago was that?
Debbie: 10 years maybe?
Allen: Yeah, I think yeah. So you’ve just become natural at using the word proxemics, a word that I don’t think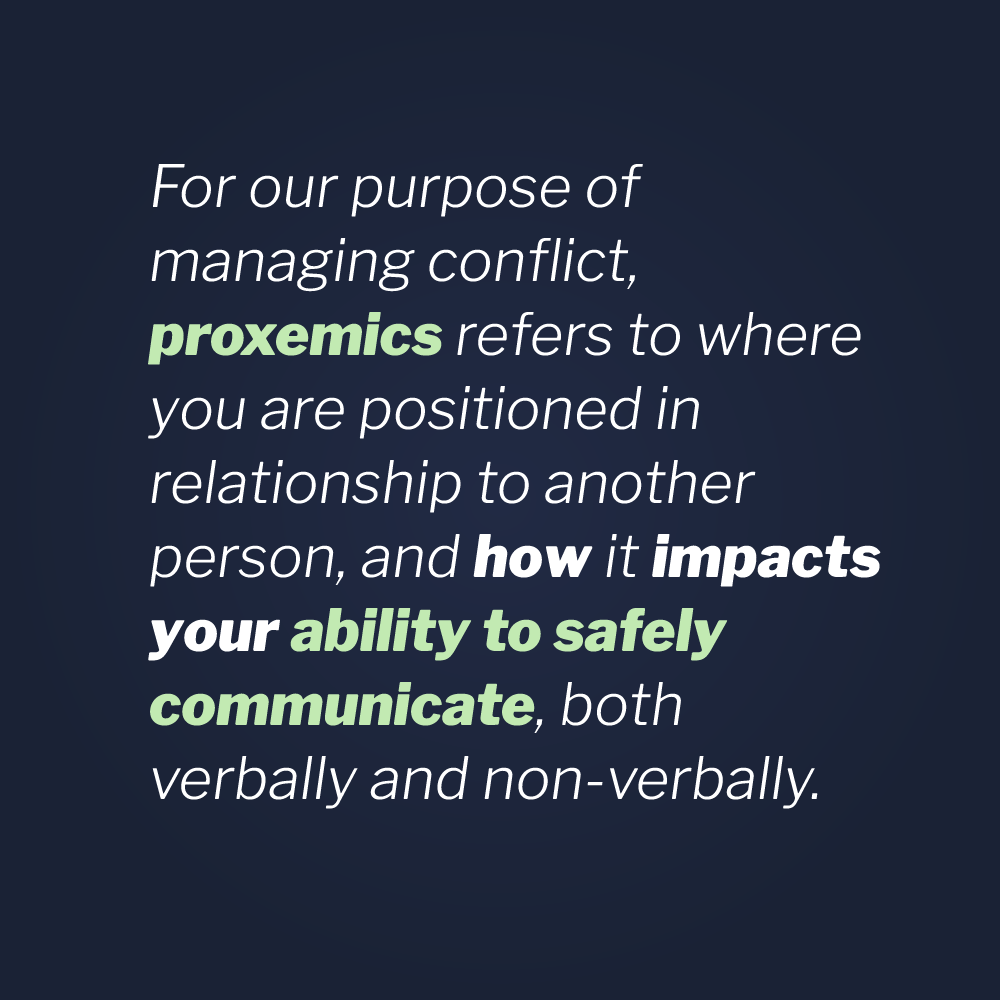 most people use. It’s like the big mystery word. But we use that word, for everybody that’s listening, as a single word that defines how your body, presence wise, related to other people in the room. So it’s your hand position, it’s your distance, it’s your physical positioning. It’s all that positioning stuff related to other people. So when Debbie says “I was paying attention to my proxemics,” It means not getting too close, making sure her hands are up, there’s a whole bunch of detail there that we won’t go into now. But anyway, that’s what that means. So go ahead, sorry.
most people use. It’s like the big mystery word. But we use that word, for everybody that’s listening, as a single word that defines how your body, presence wise, related to other people in the room. So it’s your hand position, it’s your distance, it’s your physical positioning. It’s all that positioning stuff related to other people. So when Debbie says “I was paying attention to my proxemics,” It means not getting too close, making sure her hands are up, there’s a whole bunch of detail there that we won’t go into now. But anyway, that’s what that means. So go ahead, sorry.
Debbie: Correct, correct. And when people are angry they get very animated, they don’t think as clearly, so we were able to de-escalate the situation and we had mom just leave so that we could deal with the young lady before things got anymore heated, and figure out what the argument was and how things got started and how they got to that place within the car as mom was dropping her off. And I was part of that debrief with the young lady afterwards, and walk through and talked with her and helped her debrief the interaction that she had with mom.
Debbie: So it was just one time, one example, where we had to deal with some de-escalation, where words got heated, and feelings got heated and we had to separate and support the two. That is always a big key when you’re dealing with two people who are kind of angry and argumentative, it’s getting them away from each other. And that’s why eventually we directed mom, “Hey, why don’t you just get out of here, let’s separate, go home and work this through, we’re going to work with your daughter here. And then in your next family session, you can process with your therapist what happened in this interaction.”
Allen: You use the term empathy, and as you know we’ve been talking about empathy forever, that’s a core part of our teaching. It kind of pervades everything we talk about. Then you define it as seeing the world through other peoples’ eyes or taking other peoples’ perspective. And I think, from what you’re saying here, trauma responsive or trauma informed, it’s just a deeper level of empathy. It’s really trying to not just see the world through the other person’s eyes, but see the world through the other person’s eyes based on your understanding of their background and where they’re coming from and their history and their childhood and whatever. And the more you know about that, which obviously in a residential treatment center you knew, the more empathetic you can be. Is that a fair statement?
Debbie: Yes, I think that’s a very fair statement. And it’s really that understanding of how their past trauma and things that they have gone through kind of affect their current behavior. And helping them understand that, and helping them develop some coping skills. Knowing that they have this traumatic past and that that past can affect your behaviors today, but you can also learn some coping skills of how to deal with those feelings and those behaviors. And it’s really the adults … When you’re working with young people, understanding it and really shifting our perspective to focus a little bit more on the trauma and the empathy, than so much on the behavior itself.
Allen: Exactly.
Debbie: Old school behavior management and how it was when I first started in residential treatment was really focusing on changing the behavior. And trauma informed care says “You know what? We still want to do that, but we want to do it in maybe a different way. And we want to be a little bit more sensitive and responsive to the fact that they’ve been through some trauma, and they may need things explained a little bit different or some more time to comprehend some direction.” Or things like that, and really being mindful of that. And giving them time to tell their story. When we started the debrief with the young lady, “Tell me what happened.”
Debbie: Instead of starting it out with focusing on her behavior and the fact that she was using some pretty profound, rude, disrespectful language. Back in the day, that’s where we would have started our debrief with her. But being trauma sensitive, being trauma responsive, it was more about “Tell me your story. Tell me what happened. How did you get to that place in the car where we came in? How are you feeling?” And really going at changing the behavior in that direction, versus just focusing on the behavior. And being sensitive and responsive to the trauma that she has in her history.
Allen: We talk about listening, and you just said “We’re going to ask some questions, we’re going to listen,” As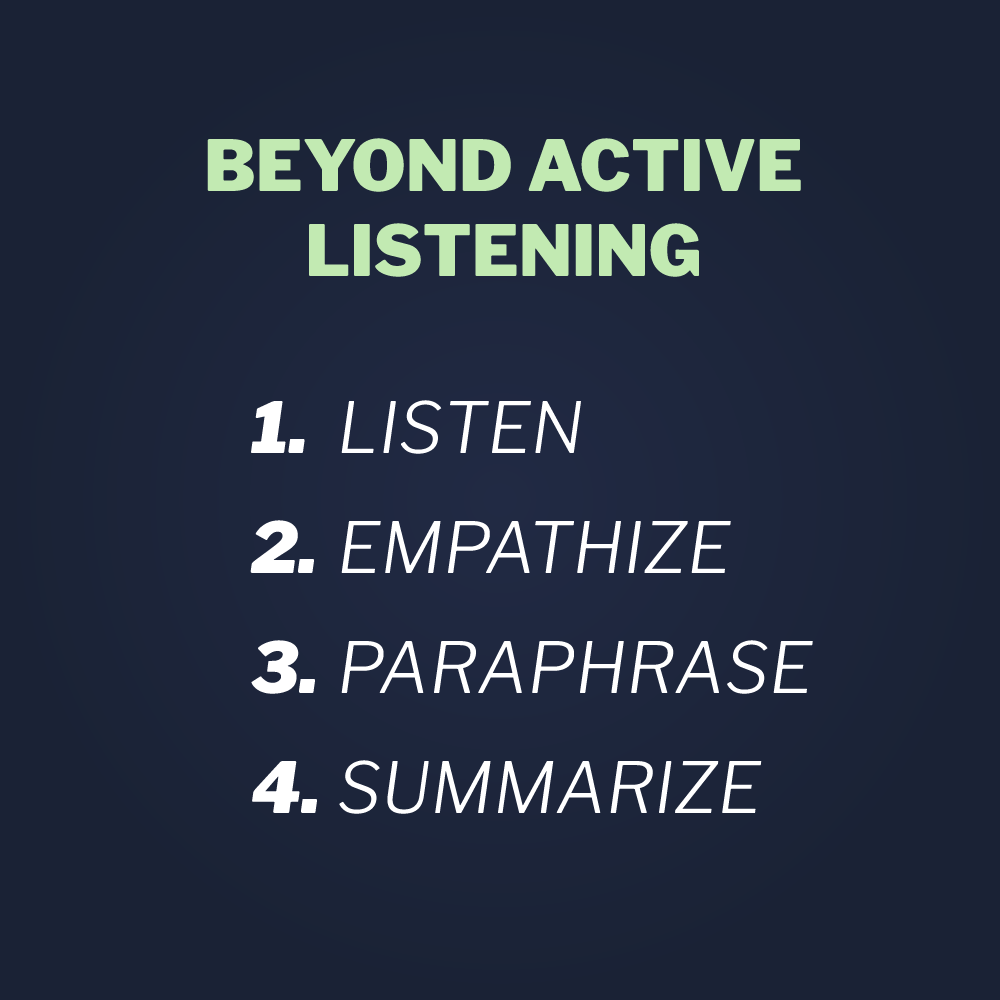 you well know Debbie, and then we talk about the fact that when there’s conflict, listening is not sufficient and then you got to go what we call beyond active listening and we have a whole series of tactics on how to do that to really … But you described some of that there, but how do you get really inside a person and understand where they’re coming from? But then we call that active information gathering, because at one level you’re calming the situation down just by being a good listener, but you’re also learning a bunch of information that then you can use to further de-escalate as the debrief continues. You’re learning about where did this come from and what are the issues and how are you feeling, and if you’re really being a very active listener and using our tactics for going beyond active listening, you’re going to learn some stuff.
you well know Debbie, and then we talk about the fact that when there’s conflict, listening is not sufficient and then you got to go what we call beyond active listening and we have a whole series of tactics on how to do that to really … But you described some of that there, but how do you get really inside a person and understand where they’re coming from? But then we call that active information gathering, because at one level you’re calming the situation down just by being a good listener, but you’re also learning a bunch of information that then you can use to further de-escalate as the debrief continues. You’re learning about where did this come from and what are the issues and how are you feeling, and if you’re really being a very active listener and using our tactics for going beyond active listening, you’re going to learn some stuff.
Debbie: Oh, absolutely. And when they’re dumping all of that or venting all of that, that’s exactly what you want to be doing. And sometimes we, as caregivers, social workers, youth care workers, we want to fix the problem for them and we want to give them all the solutions. And really, if you’re being trauma sensitive, you want to listen. You want to ask the question, “Tell me what happened.” And then you want to step back and use your active listening skills and really listen with all of your senses. What are they saying, what are they looking like? What is their body language telling you right now? And yeah, you’re really gathering some information to further the debrief, because they’re just kind of dumping it all out.
Debbie: But you can get a lot of information as they’re dumping, so to speak, to help you with that debrief down the line and further in the conversation. And when you start talking about strategies and “How are we going to look at this differently next time?” Or “What’s it going to look like when you and your Mom come together next time, how are you going to do things different?” You can start paraphrasing and rephrasing that information back to them through that conversation.
Allen: And there’s one other little thing you said there that I want to expand on just a bit, is when you said “We needed to physically intervene.” And as you know at this [inaudible 00:32:51] we talked about addressing the entire spectrum of human conflict. So there’s obviously the upfront stuff, we call it non-escalation to keep things from preventing conflict from recurring, then the de-escalation which you obviously have to deal with here. But at some point, there can be physical engagement, and you need to make a decision. Am I going to get engaged or not? One choice is to, we call it take appropriate action, but to call 911 or call your supervisor or get more people there or whatever, but in this case you decided that you needed to engage. So describe that briefly. How did you make that decision, and then what did you need to do? And I know you’ve had all the physical engagement training that [inaudible 00:33:32] offers, so just expand on that just a bit.
Debbie: Yeah. I would say in this situation it was really more low level physical intervention if you will. We were separating and supporting, we were standing between them but at a good distance. Again, using the separating and supporting. We were having good eye contact, I got some other staff involved. So one of the staff, I happened to be with the mom, and we had another staff that was dealing with the young lady. We were trying to get them to focus on us instead of each other, and I did that with the mom by continually using my verbal skills too and reminding her, “This isn’t what we want to do.” Giving her some options and saying “You know, I’d really like for you to get back in the car, I think that’s your best option, otherwise we may have to get law enforcement involved and we really don’t want to do that. We want to keep you safe, we want to keep your daughter safe.”
Debbie: Because that’s a big part of what we do at the treatment center, is keeping people safe in our job, was to keep that daughter safe. And we were not going to allow an adult, even if it was her mother, to physically harm her at that moment. So it was a lot of separation and guiding them with our bodies to separate, and getting the mom to agree to get back into her car without physically forcing her in her car, and to get the daughter to agree to go into the building with the staff to separate them from each other so that they could calm down.
Allen: I want to make sure the listeners didn’t miss the fact, and you mentioned it in your story, but you weren’t by yourself. You had already gotten other staff members with you.
Debbie: Yes, yes. Before I even walked outside, I had alerted the receptionist who was right there. Because I wasn’t sure where this was going to go. And I said “Could you just call some staff down, just have them hang in the lobby until they notice or they see from me that there’s some more help needed.”
Allen: Yep. And then was this all then separating, supporting, getting between, all that kind of thing, and maintaining distance? Or was there any point in this little exchange where you physically touched the daughter or the mom? Do you remember?
Debbie: I don’t believe I ever put my hands physically on the mom, because she was very verbally explosive, but she was listening to direction. The other thing that we were able to use is the car was right there, so we were kind of circling around the car to use the car to keep some distance between her and her daughter. Because they couldn’t get through the car, obviously, they kept having to go around the car. So it was a lot of movement and using that movement in a safe way to keep everybody safe.
Allen: Yep. Well, and that’s kind of the key message, right? And we say the best way not to get hurt is to not allow yourself to get in a position where you could be hurt. So having things in between you and the other person, separating, having multiple people there. Like you’d said, already getting that additional staff there, separating … It sounds like a verbal, you know, “Let’s separate each other, why don’t you go back in the facility, why don’t you get in the car?” That’s all in an effort to say we don’t … And it’s kind of one of the conclusions, where you didn’t actually have to touch anybody and there was still a positive conclusion.
Debbie: Correct, correct.
Trauma Informed Care Coaching
Allen: Yep. Very cool. This is great. Just maybe one more question about this coaching. When you were doing this trauma informed care, is I think what you called it as a coach, what were the number one issue that you have to deal with with people that they just didn’t get that they need to get over to start being better at this?
Debbie: I think the major issue was just to see it in a different way. Most of those folks had heard about trauma informed care and most of those folks were dealing with it with their clients, but we were really asking them to look internally and look at your coworkers and look at your policies and procedures, and look at how you treat each other. Because what we were finding also when we talked to folks in a lot of different disciplines as we’re doing training, is the coworkers are a big piece of where a lot of conflict happens. So we really wanted to have them shift their focus a little bit onto their work environment and their coworkers and their lobbies and how that looks for people who have had trauma histories. And really looking at your workplace and being mindful that coworkers and staff have trauma also.
Debbie: And it’s probably even a higher percentage in social services, healthcare, education, because that’s why a lot of people get into those fields. Part of the work I did was I worked a lot with the youth care workers in structured training, but also just kind of day to day training and interaction and interviewing. And most people when I would, you know, “Why do you want to be a youth care worker, why do you want to work with adolescents?” It was a lot of “I want to give back. I was there as a young person. I’m a caring person. I like to help people.” So by nature, a lot of people in these fields have some trauma history because they’ve been through it and they want to give back and they want to help and they get it, and they are interested in that and they appreciate the help and support that they got and they want to move that forwards, so to speak.
Debbie: So with that kind of foundation in those disciplines, it was important to talk about that. Because again, just within the average population, there’s a pretty high percentage of people who struggle with ACEs. And there were some of the teams that I was coaching that actually did that and had their staff fill out the ACE assessment and looked at it. And the results were fairly surprising. So it was really that concept, I think, that was the biggest challenge and hurdle to get people to understand, is we’re not talking about this about your clients, we’re really wanting to look at, internally, the staff and the culture within your agency. And to get that buttoned up and done well and understood. And therefore, the hope was you would do better with the clients.
Allen: Very, very interesting. Anyways you know Debbie, we ask the question a lot of, do you deal with conflict in your life? And everybody obviously raises their hands, and then the question is, is that conflict mostly with your clients, people outside the organization, or with coworkers? And almost universally, the greater level of conflict is with peoples’ coworkers. And I think you need to recognize that. And then we trained everybody at a mental health facility, all the staff, all the nurses, all the social workers. And I think probably the greatest thing we learned in that process was the fact that, just like you described, obviously you needed to be concerned about the trauma of the patient or the client, but it was understanding that the people in the room that were being trained had trauma. And that they-
Debbie: Absolutely.
Allen: That was I think a big revelation for us, and it’s for all the reasons you described, right? Yeah.
Debbie: Absolutely. And we also found that people really thought they were managing it well, and they were, until they got put back into a setting where it was kind of in their face, so to speak, on a fairly regular basis. If you’re not around it, and part of healing is to be around supportive people and be around a positive culture, and for a lot of the adults, they had done that and were in the process of doing that. But then when you came to work, so to speak, and saw it every day right in front of you again, there were some challenges there. A big part of what I did also was not only spend a lot of time dealing with crisis management with our residents, but also dealing with the youth care workers and helping them get an understanding of where they were themselves with their own stuff, and was that or was not that affecting them at work? So we did a lot of debriefing for staff and for clients after conflict happened.
Allen: Yep. And Debbie, we’ll put in the show notes a link to … And I’m sure there’s a bunch of these online places, but where you can take a peak at the ACE examples and maybe take …
Debbie: Yeah. The CDC website is probably the best. I mean, if you Google trauma informed care, trauma sensitive school, you’re going to come up with thousands, probably, of places you can get some information. But the actual ACE study is on the CDC website, yes.
Allen: And those 10 elements are right there, and it’s very easy [crosstalk 00:43:53]
Debbie: Yes, and that assessment is free to anybody. You can print it right off the website, you can print as many copies as you want. It is open and free for anybody to use.
Allen: Yep. We’ll definitely include that in the show notes. Debbie, this was great. I learned a lot, I’m sure the listeners did. This is a big area. This is not going away. It seems like when I just read the lay press that this whole concept is coming up more and more again. It’s, in effect, the post traumatic stress syndrome is effectly the same thing, right? I’m sure that’s an ACE that happens later in your life. But anything like that that creates trauma, it actually has impact in whatever’s going on in the brain, and it has long term effects. And we’ve got to be aware of it.
Debbie: Oh, absolutely, and I think the large news stories that we’re hearing now definitely can be traced back to some ACEs if you look at the people involved in the school shootings and a lot of the violence happening in the communities and the car thefts here in the city of Milwaukee and a lot of the driving issues and anger and stuff that’s going on in these communities, a lot of it you could trace back to trauma. And I would bet that a lot of the people involved in those have some pretty high ACE scores and they’re just really struggling with how to deal with all of that trauma.
Allen: Very interesting. Okay Debbie, well I’m sure we’ll do this again. Great to have you on, and probably I’ll see you later today.
Debbie: Sounds great.
Allen: Okay, thanks so much.
Debbie: You’re welcome.
Allen: Take care.
Debbie: Have a great day.
Allen: Bye-bye.


.png)



.png)
.png)