Enjoy this excerpt from one of our published books.
Chapter 6
"I Know You are Upset, But..."
Redirections, Persuasion Sequence
“Don't raise your voice, improve your argument.”
-Bishop Demond Tutu
I was engaged in a heated exchange with a man who was denied visitation by the patient herself, his own wife. She had made clear her wish not to see him and asked that he not be allowed up to her room. His expressions ran up and down the scale from disgust, to disbelief, to anger. Outwardly, he shot up and down the emotional scale from crying to threatening.
“This is really stupid! You can’t stop me from seeing my own wife!” he lamented.
“I appreciate that you feel that way, Sir, but I’m not stopping you from seeing her, she is. She doesn’t want to see you right now,” I replied.
“Can you just let me talk to her on the phone?” he pleaded.
“I wish I could, but she refused to take any calls from you,” I answered.
The exchange went on that way for minutes, with him pleading and providing excuses; and me just acknowledging his objections and redirecting his thoughts to logical conclusions.
“I’ll just go up there anyway, you can’t stop me!” he threatened.
“I understand you’re angry, but that will just make things worse for you. I can’t just let you run up the elevator and start fighting with your wife. Do you think she will be less angry with you if you cause a scene? Will you cooperate with me or do I need to just call for back up?”
At that the man looked me straight in the eye and blurted, “Yeah well, you’re fat!”
I just looked down at the potbelly that was straining the buttons of my shirt and smiled. Then I looked up at him and simply said, “Really? I’m glad you said something. Maybe we caught it in time. I better get a gym membership.”
Then the man just shook his head and chuckled, saying, “Okay, okay, you win. I’ll talk to her later when she’s not being such a b***h.”
Communication breakdowns lead to conflict and violence. An engaged response is a give-and-take process that leads to resolution. An active verbal engagement may be infused verbal resistance. Even if you’re in control of your own emotions and engaged in problem solving, your patient may not be there yet. Cursing, disagreement, challenges and disrespectful comments may be directed at you. Illogical explanations or solutions may be offered. Questions may be prompted by emotion or by someone just trying to be difficult. Excuses may be offered or even implied threats. All of these very natural distractions tend to derail communication and generate verbal resistance. The goal is to excise the emotion.
Conflict Triggers & Redirection
We are all human and certain things just make us angry. Motivated difficult people will find your weak spots or "Conflict Triggers” and exploit them in an effort to knock you off balance and take control of the clinical relationship. In the medical profession, all of us are just trying to provide the best treatment and environment of care for patients. When all you are trying to do is help, why is it that you sometimes encounter resistance? Police officers face this dilemma too. All professionals face this challenge. The strategy is to build Trigger Guards over your Conflict Triggers so they can’t be so easily exploited. By recognizing your triggers ahead of time, by identifying what offends you, infuriates you, or just plain drives you crazy, you can be ready for them when they pop up.
The best way to handle these Conflict Triggers is to use the Redirections tactic. The “I know you are upset, but can you work with me?” approach is the formula for diffusing and disempowering any emotional assault. Redirections come in many forms like the humorous example above. But they also come in the form of pre-planned, practiced responses like the examples below: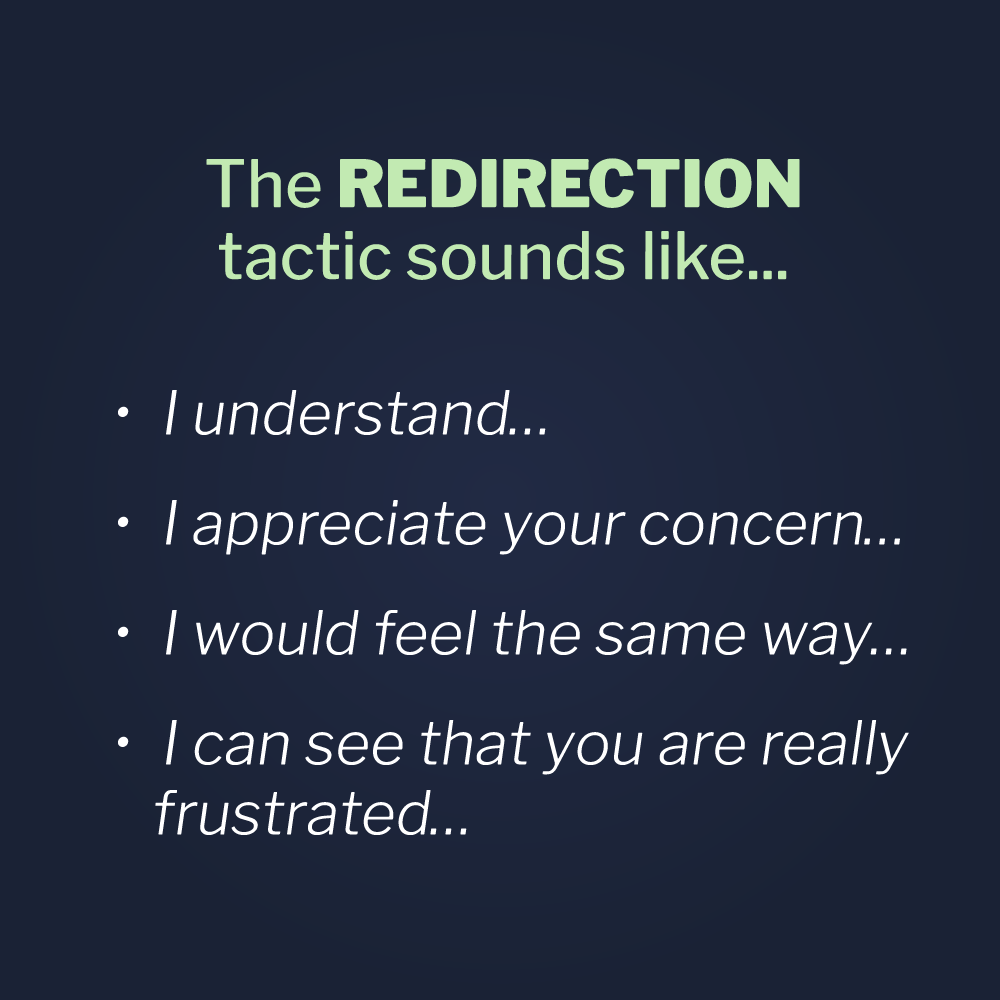
- I understand…
- I appreciate your concern…
- I would feel the same way…
- I can see that you are really frustrated…
Statements that begin in this way intercept negative comments and acknowledge them in a positive way. As any boxer or martial artist knows, deflecting a strike not only protects from injury, it also provides a positive opportunity. Acknowledging a person’s comment is especially powerful if used in combination with Empathy.
- I see that you are upset and I appreciate your concern…
- I know this must be difficult for you and I can hear that you’re worried...
The Redirections tactic is given context when the acknowledgement is immediately followed up by redirective language. The words “but” or “however” help to transition to solution-oriented language and help focus on problem solving rather than problem creating. Below are some examples of what we’re talking about.
- I know you are upset, but…
- I can see your concern, however…
- I know you are frustrated and maybe I would feel the same way, nonetheless…
The solutions then offered might be as simple as…
- …could you please work with me?
- …would you help me help you?
- …we need to wait and see what the doctor thinks.
Putting this all together, Redirections end up sounding like this:
- I can see that you are upset but we need to wait until the test results come back and that can unfortunately take up to an hour. Can you work with me here?
- I know this must be difficult and I would probably be upset too under these circumstances. However, if you will work with me we can make sure that your child gets the exact care he needs.
Redirections are a way of inserting a tactical pause in a situation before our emotions over-ride our intellect. Childlike tantrum behaviors are only fed by childlike behavior in return. Our adult response, with the proper tone that is not authoritarian but caring, coupled with our calm response and demeanor, can re-assure the most emotionally out-of-control person that we are in control and can help.
I was sent to the nursing unit one night because a family court in another jurisdiction had requested that our hospital take temporary physical custody of an infant who was being treated for suspicious injuries. The baby had been flown to us by medevac helicopter from a neighboring state. The state had also faxed over the court order taking custody of the child. After meeting with the hospital manager on duty and the unit supervisor, the task fell on me to inform the baby’s mother. I called the Child Protective Services agent involved in the case, to get specific instructions and prepare for the conversation ahead of me. It would turn out to be one of the most difficult conversations of my career.
When I arrived at the room it was dark, as only the light above the vanity was on and glowing dimly through the narrow window on the door. I knocked, but there was no answer. Slowly cracking the door, I could hear the mother weeping softly somewhere in a dark corner of the room. The nursing staff said she was alone, so I opened the door a little wider, stood in the doorway, and began with a Universal Greeting.
“Hello Ma’am, my name is Joel Lashley, I’m the Supervising Security Officer on duty in the hospital tonight. The reason I’m here is to inform you of where we are in the investigation concerning your baby’s injuries.” She started to sob openly now, so I took a deep breath and continued. I tried my usual practical appeal, by looking over at the crib and asking, “How is your baby resting now?” She didn’t answer but only continued to sob deeply.
“I know this is very difficult, but I have to explain what’s happening. Your state has taken temporary custody of your child and placed him in our physical custody until our doctors can complete their evaluation of your baby’s injuries. Until then, you will not be able to visit. You have a court date on Monday that I need to tell you about and I have some paperwork to give you.” The young mom began to cry openly now, so I just continued slowly and gently. “Your baby is safe here with us. He will get all that he needs and you can call whenever you like to get updates on him. If you have any questions for the nurses before you go, they will be happy to answer them. No decision about your child’s future custody has been made yet. You just need to cooperate for the time being, as these things take a little time.”
Just then, a fierce looking woman, who turned out to be the grandmother, pushed passed me and into the room. She went directly to the crib and picked up the sleeping baby, causing his IV lines and monitoring wires to dangle from his limbs in a tangled mess. “Ma’am, please put the baby down. He’s injured and you don’t want to make things worse,” I said.
“No one is taking my grandchild from us!” she shouted as the baby began to cry.
“No one wants to take your baby, Ma’am, but he has to stay with us until things get cleared up…”
Interrupting me, she blurted, “We’re leaving!”
“Ma’am, we have a couple good options here. You can put the baby down and, with the mother’s permission, I can answer any questions you have. But, if you insist on trying to leave with that baby, I’ll have to stop you. If you struggle and injure the baby, you’ll be arrested.”
“I don’t care!” she shouted.
“Also, I have to file a report on how things go tonight. I want to write that you were concerned about your grandchild’s health, asked a lot of questions, and cooperated with us. I don’t want to write that you fought with us and manhandled the injured baby. What do you want me to write, Ma’am? It’s all up to you.”
After a few seconds of processing what I just said, the grandmother started to gently place the baby back in its crib. “I don’t know who you think you are,” she said, while still cooperating. “Do you feel like a big man taking people’s babies away?” Just then the baby’s father and grandfather walked in the room. The grandfather started in by saying, “What the hell is going on here?”
At that moment, the baby’s mother said her first words, “Stop! All of you stop and leave him alone! He’s the only person, since all this happened who hasn’t treated me like a criminal!” Ultimately, the family cooperated and did just as I had hoped for them. They asked a lot of questions, showed their concern and love for their baby, and cooperated with the terms of the court order. Before leaving, the father and grandfather thanked me and shook my hand. The mother even gave me a hug.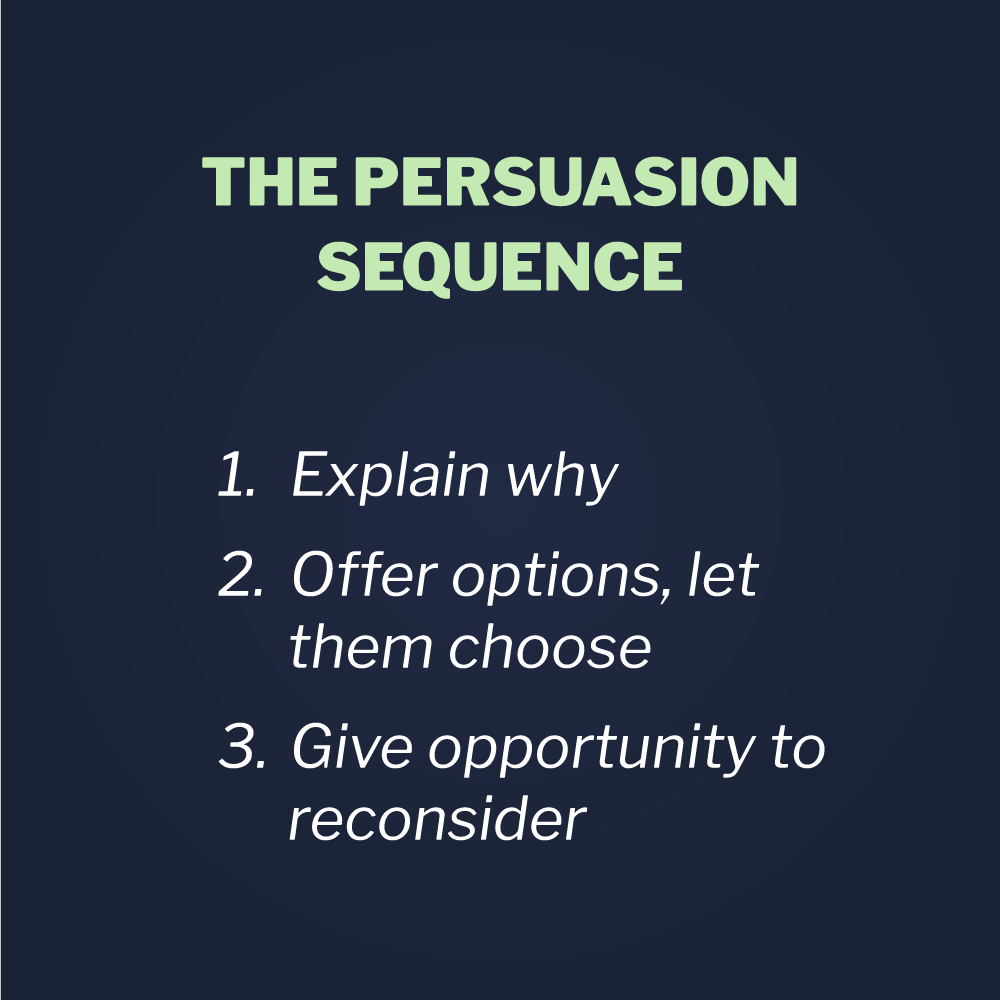
The Persuasion Sequence
The story above was an example of Vistelar’s Persuasion Sequence in action. First, by beginning with a Universal Greeting, I was able to establish communication with a young mother in distress. Then when resistance was encountered I was able to manage the contact, by use of the Persuasion Sequence. First, by asking the grandmother to comply by putting the baby down and then by setting context for her, in other words, telling her why it was in her best interest to cooperate. Finally, I was able to generate voluntary cooperation by presenting the options; thereby, helping her to understand her choices, both good and bad. The options stage is in a very real sense, a reality check. In the majority of cases, even when under stress, most people will take the best option offered to them.
The genius of the Persuasion Sequence is that it causes both the provider and the patient to think clearly under pressure. That’s because speech is a psychomotor skill, just like a golf swing. Through proper modeling, followed by practice and repetition, muscle memory is achieved. Once ingrained, the Persuasion Sequence provides a cognitive template, by which both patient and clinician can think clearly even when angry, frightened, or confused. The clinician is guided by their training and the patient is guided by the professional presence and voice of the provider. It’s as simple as that.
Through proper modeling, training and practice, healthcare professionals can become proficient crisis communicators. In the majority of cases, a well-done Persuasion Sequence is effective even in seemingly impossible situations. Later in my career, I succeeded so often using the Persuasion Sequence that I was actually surprised when people didn’t cooperate. At the beginning of my career, especially before training in Vistelar’s conflict management methodologies, I was more often surprised when they did cooperate!
That may have been partially a function of experience; however, I’ve known many police officers, physicians, and supervisors who struggled their entire career, by never getting much cooperation from the people they served. In my own case, I believe my poor communication skills early in my career were a function of four dynamics: 1) A lack of experience. 2) A misunderstanding of my role, believing that my job was simply to enforce the rules. 3) The ingrained belief in healthcare that patient or family centered care is incompatible with setting limits on bad behavior and enforcing polices — even the law. 4) Training based solely on de-escalation theory instead of including non-escalation and Crisis Intervention concepts.
That said, even in the rare instances when things didn’t end as I’d liked, the Persuasion Sequence demonstrated that everything possible was attempted to convince the subject to cooperate and that subsequent appropriate action was justified. Gary Klugiewicz, from Vistelar, often puts it this way: “The point is to at least look good, no matter how things end up.”
A common example of the “looking good” benefit of the Persuasion Sequence might be when we are forced to Take Appropriate Action if patients or their family members are disruptive. In a few cases, physicians who were rightly advocating for their patients demanded answers for why their patients or their visitors were expelled. One conversation I once had with a provider went like this.
“You mean to tell me that you threw my patient’s mother out of the hospital? Are you crazy?!” complained the doctor.
“Yes Ma’am, I did. I asked her to leave because she was disruptive and disturbing other patients on the unit.”
“Well her kid just had surgery, for God’s sake!” she said tersely.
“I understand that, doctor, but the kids on either side of her room also just had surgery.” After using the Redirections tactic, I simply continued building context. “Their parents were complaining and one of the other kids was crying and upset because of that mother’s behavior. Her actions were affecting not only her own child’s recuperation, but that of other kids on the unit.”
“Well couldn’t you just have asked her to stop?”
“Oh I did just that, doctor. After I introduced myself, the next thing I did was ask her to stop yelling and cursing on the unit.”
“What did she say?” she asked.
“She said ‘F*** you!’ loud enough for the whole hospital to hear,” I replied.
“Okay, did you explain to her why she couldn’t do that?” asked the doctor.
“Absolutely, I explained that she was frightening the other kids. I said I understood that she was angry and that I wanted to help her out.”
“So….then what did she say?” asked the doctor, now in a much softer tone.
“Well, she said she didn’t give a s**t about anyone else’s kid and just kept threatening and cursing.”
“Okay, so is that when you threw her out?” asked the doctor, sheepishly.
“No, not just yet. First I offered her a choice. I advised her that, if she stopped yelling, I would do whatever was in my power to help her out. I even offered to get a nursing supervisor and a quiet conference room we could use, so as not to disturb other patients.”
“Really?” asked the doctor.
“Yep,” I replied. “It’s all in my report. But she just kept it up. She said she didn’t want to discuss it and continued cursing and yelling at nurses and even at visitors as they walked on and off the unit.”
At that, the doctor simply said, “Okay, okay I get it, you had no choice. That’s when you threw her out.”
“Nope,” I said.
“Really? Why not?” she asked wearing a surprised expression.
“Because I wanted to give her an opportunity to reconsider. Like you say, her child just had surgery. So I asked if there was anything at all I could say to get her to stop causing a disturbance, and she yelled, “F*** you and this f***ing hospital!” at the top of her lungs. At that point I didn’t have any choice but to escort her off the unit.”
“Well, I guess you had no choice. So was my patient upset that his Mom was ejected from the hospital?” she asked.
“Well, he might have been and sometimes kids are upset when this happens. But in this case, I honestly think he was relieved.”
So, as we’ve seen, the Persuasion Sequence not only makes us more effective communicators, but also effective behavior managers at the point of impact. We also are able to use it justify our actions.
Again, before using the Persuasion Sequence you must ask. Just as in the Big, Mean, Angry Biker story, we focus on behavior hoping to affect the attitude and generate voluntary cooperation. In the case of a gateway behavior like cursing in your facility, a Persuasion Sequence might need to be used after asking, “Sir, could I please ask you to stop cursing?” and not getting cooperation.
That is an example of an initial way you might approach things. Your expression should reflect concern and your tone of voice should be supportive and professional. In this way, you present your on-stage face (Showtime Mindset) to your patient. As Gary Klugiewicz often says, “the goal is to first create a reasonable doubt in their mind that you are not a jerk!“ First impressions are everything. Once you’ve asked someone to do something, you should always offer the reason you’re asking. Telling someone “it’s the rules” or “because I asked you to” is a very natural response. But, as with most natural responses, they rarely work.
People want concrete reasons when you ask them to cooperate against their own judgment or when asking them to modify their behavior. “There are little kids around and they can hear you cursing” is a real-life explanation of why cursing, yelling, or threatening may be inappropriate. Also, trotting out your hospital’s policies is rarely effective when not placed in proper sequence. Policies and laws can be effective in locking down context, however, after an explanation has first been offered. “Also, hospital policy does not allow cursing because this has to be a safe and appropriate environment for kids and families” is another way to set complete context for people who are resisting your attempts to address their behavior.
Once clear options are presented and people are given ample opportunity to cooperate, most will choose to go along with the program. For those who refuse, presenting them with their Options, or in other words Choices, is your next step. “Sir, we have a couple good options. You can stop cursing and I can try to help you out. I really want to help with whatever your situation is. But, if you insist on cursing in the hospital, I’ll have to ask you to leave.”
At this stage, it’s very natural just to threaten, “If you don’t stop, I’ll call security.” Threats never work. They are just challenges that beg to be taken up. If we were to start with the bad option first, the third step in the Persuasion Sequence always sounds like a threat. A bad example might be, “Sir, I can call security or you can just stop cursing and go about your day.” Again, through training and practice, providers learn to offer the options in a professional and effective manner. By practicing saying prompters like, “We have some good choices,” reminds us to start with the good options and avoid sounding threatening or authoritarian.
It's Not What You Say, But How You Say It...
In the case below, a clinician sets limits while using a noticeably quiet volume and softer tone.
Clinician: “Mr. Johnson, I know you’re upset and I want to help. We have a couple good options. Just stop yelling and we can get to the bottom of what’s bothering you, or let’s step over to the conference room so we’re not disturbing the other patients. But, if you insist on yelling and cursing in the clinic, I’ll have to ask you to leave. Can you work with me?”
Mr. Johnson: “You can’t kick me out, I’m sick!,” he replied urgently, but less loudly this time.
Clinician: “I don’t want you to leave. You need to be here with us. We want to get you well and start feeling better.”
Mr. Johnson: “Then help me.” He asked now at a normal volume, following the clinicians’ tone down to a safer place.
Clinician: “We are helping you, Mr. Johnson. We checked your vitals and you’re safe with us. Sit right here where we can keep an eye on you. The bathroom is right over there and you can’t have any water right now, until we know exactly what is wrong with you or you could get sicker.”
Mr. Johnson: “Why can’t you just see me now?” he pleaded. Clinician: “Because you are not the only sick person here. Some of these people have been here longer and a few of them are sicker than you are. Do you want me to make them wait longer to see
you first?” Mr. Johnson: “No.”
Clinician: “Okay. I’m glad you understand. Honestly, unless someone comes through that door with a heart attack, we will see you within the hour. Let’s just keep our fingers crossed. Okay?”
Mr. Johnson: “Okay.”
Non-verbal communication is just as important, if not more important, than what you say. Again, providers have the position of advantage in every situation where they are communicating with patients, families, or visitors, unless they choose by their actions to surrender it. In this case, the clinician gave clear options and empowered the patient to make the choice. She also locked down context by giving clear and concrete reasons why he couldn’t be served immediately. Lastly, she modeled the behavior she wanted to see from her patient.
When we are challenged, our natural instincts are to match the tone and volume of the aggressor or clam up and shrink into a posture of submission. Neither approach is safe or productive. By “Reverse Yelling,” we can reset the pace and volume of the conversation, causing the aggressor to follow us down to a quieter, calmer, safer level. All behavior equalizes. The person with the best communication skills sets the tone.
Reverse yelling is just another one of the psychomotor skills, like Proxemics 10-5-2, that practitioners of Vistelar’s conflict management methodologies develop as they practice their skills in training. By sticking to the basics in scenario-based drills, they not only begin to master basic communications skills, they also build confidence that will guide them through conflict on the job, at home, and in their daily lives.