Enjoy this excerpt from one of our published books.
Chapter 3
Visiting Hours are Over:
Showing Respect, Showtime Mindset
“An eye for an eye will make the whole world blind.”
-Mahatma Gandhi
In my career I’ve worked in several healthcare facilities, including everything from large urban hospitals to sub-acute centers located in the heart of street gang territory. Many years ago when I was training for a job as a hospital security officer, I was shadowing another officer to learn the procedures at a visitors’ desk.
Our assignment was to greet everyone attempting to enter the main entrance to the hospital, after visiting hours had ended. We were to determine why they were there, give them a visitor’s pass, and direct them to their destination when appropriate. That part was easy. The difficult part came when we had to tell people that only immediate family were allowed to visit after hours and that they couldn’t visit their neighbor, co-worker, or nephew. As you can imagine, no one was ever happy to get that news.
When visiting hours ended at 8PM, my training officer and I locked all the front doors except for one. Then we put out the sign, turned down the lights, took our seats, and waited. We didn’t have to wait long. By 8:15 the first would-be visitor walked right past the “Visiting Hours Are Over” sign and up to the visiting center. My training officer took the lead as it was my first day on the job. The officer greeted the visitor by simply stating, “Welcome to the General Hospital, how can I help you?”
“I’m here to visit somebody,” began the visitor.
“Okay, how are you related?” asked my training officer in a somber tone of voice.
“Uh, well, I’m not. She’s just a friend,” replied the young man. The officer replied, “Visiting hours are over.”
After a pregnant pause, during which the two men stared blankly at each other, the visitor replied, “Really? Can I just run up and say hi for a second?”
The officer looked up at the man and replied in a disinterested tone, “Well, visiting hours are over, so you’ll have to come back tomorrow.”
“That’s ridiculous,” replied the man.
“Sorry but that’s the way it is. I don’t make the rules,” said the officer.
“Well you don’t have to be a jerk about it!” fired back the man in an angry tone of voice.
After a little more back and forth, the conversation deteriorated into a shouting match. The man left in a huff, while threatening to call and complain about what he believed was the shabby way he’d been treated. Now sitting in silence, I could tell that this was not my training officer’s favorite part of the job.
By 8:30, another visitor arrived. A high-energy middle-aged woman appeared at our desk, beaming a broad smile and carrying a grocery bag full of treats, magazines, and toiletries for some hapless patient. Seeming to notice my training officer’s blank expression and lack of eye contact, she took a couple of steps over to address me instead.
“Hello. Welcome to General Hospital. How can I help you this evening?” I said.
“I need to get to the maternity ward. My neighbor is having a baby and she forgot some things at home. This is such an exciting time! It’s her first baby!” she said.
“Well how nice of you to bring her things down…” I began to say before being interrupted by my training officer.
The officer leaned over and blurted in a terse tone, “Sorry, but visiting hours are over.”
The woman nervously blinked, wearing an expression of surprised disappointment, and said, “Oh poo. Can I just run these things up to her? She has no clothes or anything. She’s waiting for them.”
“You’ll have to come back tomorrow. They have anything she will need up on the floor,” said the officer.
The woman’s expression went from disappointment to indignation. “Well, she said I could bring these things down. Could someone at least take them up to her?”
“We really don’t have anyone available to do that,“ he replied, wearing his signature expression of disinterest.
“Then can I leave them here until someone is available to run them up to her?” she retorted angrily.
“We can’t accept things from visitors. We can’t be responsible for them,” he fired back.
“I want to talk to your supervisor, this is ridiculous!” she replied tersely.
At that point the officer did as trained and called the charge nurse on the unit. She instructed the officer to issue a visitor’s pass and send the woman up. With a look of satisfaction, the woman took her pass and walked toward the elevators that would take her to the obstetrics floor. “See that?” he asked me. “Sometimes it doesn’t even pay to try and stop anyone from visiting.”
A few minutes later, a young couple and their two young children approached the desk. The kids were holding balloons and smiling happily in anticipation of visiting their cousin in the hospital. This time I stayed silent and waited for my training officer to begin. He looked down at his desk with a look of obvious frustration and said, “Welcome to General Hospital. How can I help you?”
“We need to go to pediatrics,” replied the woman in a pleasant tone of voice.
“How are you related to the patient, Ma’am?”
“He’s our nephew and these are his cousins” she replied pleasantly, while motioning towards her smiling and well-behaved children.
“Only immediate family after eight o’clock. I’m sorry,” he replied tersely, clearly frustrated by a bad start to the evening.
As you can imagine, the conversation went south from there. After a couple more exchanges, the security supervisor was called to the desk to deal with the angry couple. Soon after the supervisor and the disappointed family left, my training officer looked over at me and said in frustration, “Boy, people are sure showing up in a crappy mood tonight.”
The Challenges of Communicating As A Healthcare Professional
The main thing I learned from that training officer on my first day was how not to communicate with patients and visitors. As the evening went on, every visitor who was turned away seemed to leave with a bad impression. They not only left with a bad impression of my training officer, but of me as well. They also left with a bad impression of the hospital, as we were both guilty by association.
Healthcare is a high-stakes profession. Just as in law enforcement, many of the daily decisions that healthcare workers make can drastically affect the lives of the people they serve. If we accept that as true, then a professional’s outlook—whether they are a police officer, a teacher, or a doctor—should be such that it best serves the interest of the people who place their trust in them. That said, the routine of human service work—where professionals frequently encounter people at their most anxious, angry, or defiant—challenges the professional’s positive outlook toward the people they serve. As a result, human service professionals often develop a negative mind set towards their clients.
Criminal Justice educators and trainers sometimes refer to the 90/10 Ratio in law enforcement. The 90/10 Ratio refers to the belief that 90 percent of the people in the world are basically good and ten percent are basically bad. While most of us (the ninety percent) obey the law and contribute positively in some way to society, a smaller number of people (represented by a figure of ten percent) are responsible for most of the conflict, crime, and iniquity in the world. However, some law enforcement professionals believe that, due to daily exposures to people behaving badly, many officers flip the 90/10 ratio over to a 10/90 ratio—a point of view in which the law enforcement officer believes that only ten percent of the world is filled with good people, meaning that 9 out of 10 people are jerks, law breakers, and untrustworthy.
The 10/90 Ratio outlook is one that healthcare professionals often fall victim to as well. If that’s the case, could the belief that most of the people who walk into our emergency rooms and clinics are bad people negatively affect our interactions with patients at the point of impact? The concept is at least worth exploring.
As I worked over the next few weeks with that training officer as my guide, I learned a great deal about him. He could, in fact, be a very personable guy. He was well liked by his co-workers in the security department. The nursing staff in the emergency room liked him as well. He was funny and friendly. He got along well with everyone it seemed, except ironically, the people whom we were there to serve. He was poor with his communication at the welcome centers, on the floor, or anywhere else that he was called upon to deal with patients and families. After working alongside him for a while, I started to build an understanding of why he struggled to communicate with the hospital’s customers.
Armed with the supposition that anyone who walked past a sign that read “Visiting Hours Are Over” is either a jerk or stupid, he greeted them all with an annoyed expression and a disinterested tone. He visibly avoided eye contact with people as they approached the desk, instead looking down at his computer screen, at the counter top, or over at me. When a visitor approached the welcome center, he would offer his canned greeting of “Welcome to General Hospital, how can I help you?” at a fast pace and in a monotone voice. When challenged, he would offer no explanations, no solutions, no empathy, and no regret. He would offer none of these things with his words, with his tone or volume of voice, or even with the expression of his face.
Communicating Under Pressure
When dealing with disturbance calls on a nursing unit, or anywhere else in the hospital, he also struggled hopelessly. He rarely got compliance from people and had to rely on supervisors and co-workers to try and bail him out. When on patrol, he often looked the other way when seeing or hearing issues that should be addressed, just to avoid confrontation. Though he obviously was adept at communicating in social situations, he was inept at communicating in the midst of conflict. And he is not alone. Communicating under pressure is difficult for everyone, but it’s what we do most often as human service professionals—talk to people under pressure. Still, we spend very little time, if any, learning how to do it.
The first step in learning how to communicate under pressure is to work on the 10/90 mindset—the belief that everyone we deal with is a jerk and that no matter what we say or do, we cannot win when dealing with them. To achieve this mindset change we must begin with a better understanding of human nature.
A core principle Vistelar teaches about human nature is that everyone deserves to be treated with dignity by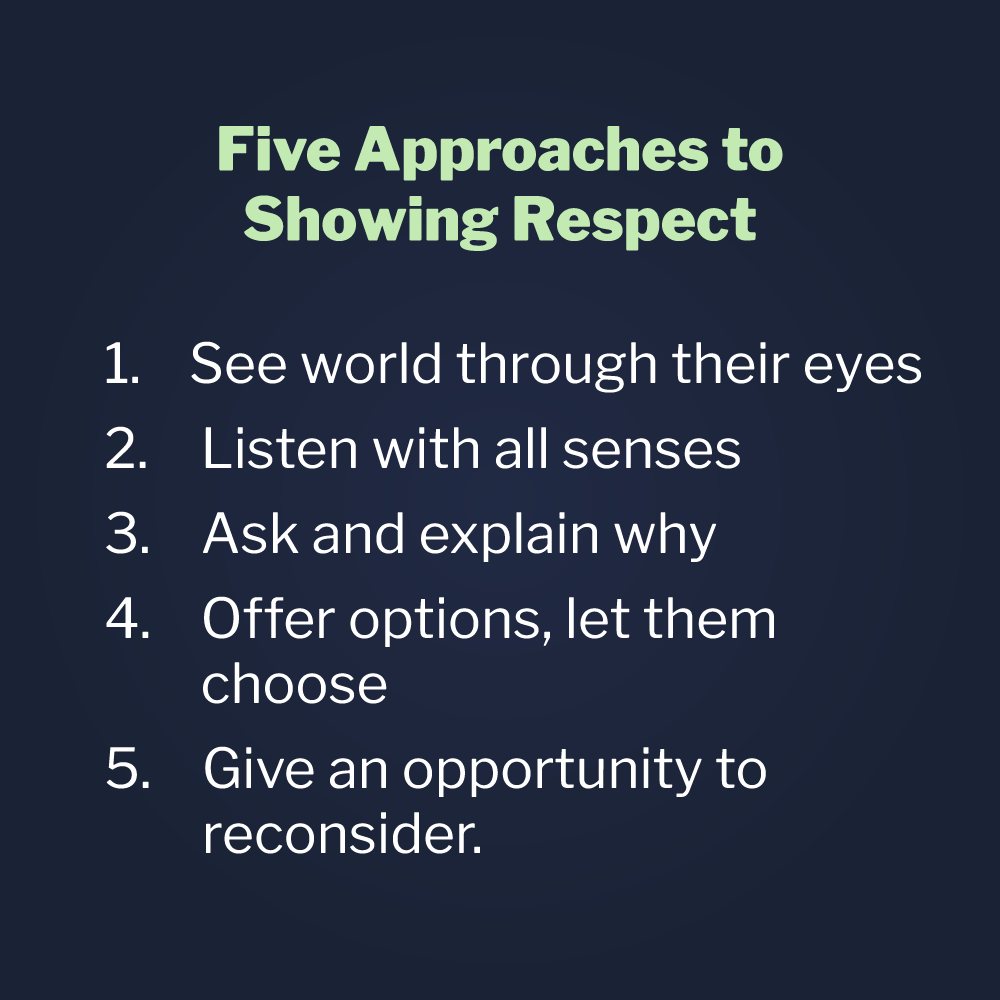 showing them respect and that, to show respect, you must follow these five approaches 1) See the world through their eyes; 2) Listen with all your senses; 3) Ask and explain why; 4) Offer options, let them choose, 5) Give opportunity to reconsider.
showing them respect and that, to show respect, you must follow these five approaches 1) See the world through their eyes; 2) Listen with all your senses; 3) Ask and explain why; 4) Offer options, let them choose, 5) Give opportunity to reconsider.
One of the best lessons I ever got on treating people with dignity by showing respect was from a co-worker. A manager in an office where I once worked decided to print and post pictures of all the important people in the company. Being a very large company, we ended up with many faces posted on our office wall. Under each of the faces of the CEO, President, many Vice Presidents and department heads, were their names, departments and titles. Almost daily, whenever he walked through our office, he would say, “Now you guys all learn these names and faces. When you see them, show them respect and make sure you are on your best behavior!” Soon, his little “respect” speech became a familiar feature of our office life.
After a few weeks of pounding home the need to respect important people in the company, he started to quiz us. He would catch some unfortunate person walking by his “wall of fame”, as he called it, and cover the title section under one of the pictures with his hand. He would then ask, “What’s this person’s name, department and title?” If we got it right he’d say, “good job.” If we got it wrong, we got dressed down. In short, he wasn’t treating any of us with much respect. In fact, he had quite a reputation around the company as being a jerk. He wasn’t well liked by much of the staff in our department or in any other department. But he was liked, however, by a lot of people in authority. Probably because he practiced what he preached.
If he bumped into someone important, he would smile and greet them in an exuberant and friendly fashion. He would call them by name and compliment their clothes or haircut. He would congratulate them on a promotion or tell them how much he appreciated their contribution to the company. His reputation, however, was very different among his own staff and other employees of the company. In fact, he was viewed by many as being unfriendly, demeaning, and rude. Some saw him as racist and sexist, and complaints were not uncommon about his attitude and behavior. Still, he plugged along happily day after day, instructing all of us to treat people with respect, as long as they were someone in authority.
On one particular day, this manager looked around the office and called over another manager to review his “wall of shame”, as it had become popularly known. He placed his hand over the title section of one picture and asked the other manager if he knew who that was. The other manager looked around at all of us in the room. On our faces he saw expressions of embarrassment, disgust, and discomfort. Then he looked at the manager and simply said, “You know what? If you would just learn to treat everyone with dignity by showing them respect, you wouldn’t have to memorize these names and faces.” By the next day, the “wall of shame” was gone. It was taken down and thrown in the wastebasket by some anonymous person and was never put up again.
If my old training officer at the hospital where I once worked had known and embraced Vistelar’s five approaches to showing respect, chances are he would have been one step closer to being as successful with the people he served as he was with the people he worked alongside. Although he resisted professional communications training (Verbal Defense & Influence) at first, over-time he embraced it as he saw others using it and succeeding under pressure. Now he is well respected, highly competent, and a hospital security leader. His former weakness had become one of his greatest strengths, as he is often sought out to have difficult conversations in difficult situations. If my old manager, with the “wall of shame”, had treated everyone with dignity by showing them respect, and not just the people in charge, he wouldn’t have lost his job, which eventually he did. He lost it because of all the disrespect he had shown and the complaints he generated as a result.
Showtime Mindset
Vistelar’s five approaches to showing respect are not only the basis for treating people with dignity but for persuading them to cooperate (which you’ll learn in a later chapter). But, for the five approaches to be successful, both the words you say and how you say them are critical. That is why it’s important to understand and adopt the Showtime Mindset.
On another occasion, I was given the assignment of protecting a social worker while she addressed the behavior of a threatening family in a hospital. We were to go to the room of a gravely ill child and readdress the parents recurring threatening language towards staff. The patient was chronically ill, experiencing frequent and lengthy hospitalizations. The parents reportedly fought daily between themselves, and cursing and yelling were regularly heard on the unit. Frequent attempts to rein in their behavior had failed and all involved were at a loss about what to do.
As luck would have it, by the time we arrived on the unit we could already hear yelling and cursing coming from the patient’s room. As soon as we arrived at the room, a fearful nurse ran out and scooted quickly down the hallway. Before arriving our roles for the intervention had been clearly defined. The social worker was to do all the talking and I was to observe and protect if necessary. The social worker walked into the room wearing a surprised expression, with me on her heels and remaining silent as asked.
The social worker began by saying in an urgent tone, “Hey, what’s all the yelling about?”
“We don’t have time for this bulls***,” replied the father. As you can imagine, the conversation spiraled out of control. When the father got louder, the social worker shouted back, matching his tone and intensity. When he accused the nursing staff of incompetence and indifference she became defensive. Soon, both the mother and the father were standing and facing off, nose-to- nose with the social worker!
Just as I was about to step in, there was a loud knock on the doorframe. After getting everyone’s attention, the Director of Security walked in. Wearing a business suit and an expression that could only be described as a concerned smile, he walked towards the parents with his hand outstretched and said, “Please allow me to introduce myself.” At that, the startled parents stood silent. Then suddenly, the father smiled brightly and took the Director’s hand, saying, “See, that’s how you come into someone’s room!”
Simply put, the Showtime Mindset refers to the necessity to always be on stage when we’re at work. Walt Disney, in all his genius, understood this concept very well. He understood the experience of the customer is always tied to presentation. That’s why you’ll never see a guy in a Mickey Mouse costume sitting at a lunch counter in Disneyland, with the head of his costume sitting next to him while he eats a hamburger. Disney understood he could never take the chance of revealing to the kids passing by that there is only an ordinary man inside that costume. He also understood that Mickey’s little secret was just as important for the adults who visited his theme park. It was Mickey, Goofy, Snow White and all the little characters that set the tone for the experience — not just people inside colorful costumes.
Vistelar’s conflict management training takes practitioners through drills that develop their Showtime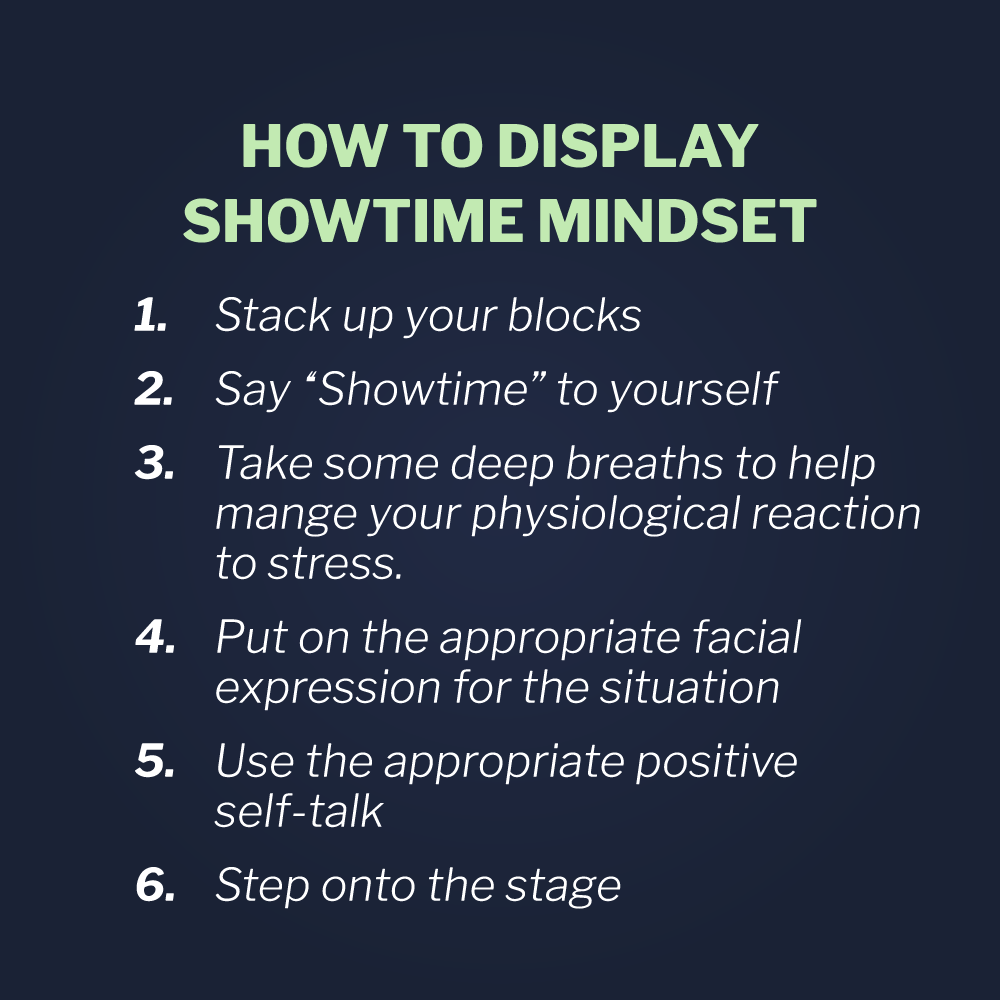 Mindset. In training, they learn to adapt their non-verbal and verbal communications skills. Habits like nervous smiling, crowding, matching volume, matching tone, and verbal overload are identified and worked on in a way that builds psychomotor skills in the learner. After all, speech and communication is very much a psychomotor skill. Scenario based training in professional communication gives the student the feeling that they’ve been there before when difficult situations arise. By building these memories in training, we can transfer canned experience to the real world. This is something that cannot be achieved in a book or video presentation.
Mindset. In training, they learn to adapt their non-verbal and verbal communications skills. Habits like nervous smiling, crowding, matching volume, matching tone, and verbal overload are identified and worked on in a way that builds psychomotor skills in the learner. After all, speech and communication is very much a psychomotor skill. Scenario based training in professional communication gives the student the feeling that they’ve been there before when difficult situations arise. By building these memories in training, we can transfer canned experience to the real world. This is something that cannot be achieved in a book or video presentation.
Managers in customer service commonly instruct their employees to smile. “Always wear a smile” is a mantra heard in retail establishments across America and generally it’s good advice. I agree that in most circumstances people need to look approachable and friendly while at work, whether they are a police officer, nurse, or cashier. That is an important part of developing a Showtime Mindset. But just as with anything else, people need more than one tool on their belt.
Appropriately Adapting Communication
Many years after my first day on the job as a hospital security officer, I was working as a communications skills trainer. I was asked by a patient representative department manager to mentor one of her information center employees. At this particular institution, visitation staff, not security officers, staffed the information centers or welcome centers, even after hours. The manager advised me that her employee was struggling in her job and had received several complaints. She wasn’t sure why, because the employee was really quite personable, but she would be forced to terminate her if complaints continued to roll in.
When I finally learned the welcome center staff member’s name, I was shocked. “Her?” I said, “She’s the nicest lady here! Everyone loves her!” This was one of those employees who was always smiling and friendly. She always offered a big “hello” for everyone who walked in the door. She always made an obvious effort to make every patient, visitor and employee feel truly welcome. Frankly, I was stumped. Unbeknownst to her, I watched her work for a few hours and couldn’t understand why she was generating so many complaints. On the outside, she appeared to be a master of the Showtime persona.
As you might expect, most of the complaints came in when she had to turn people away who were not allowed to visit or when it was past visiting hours. Finally, I scheduled myself to sit at a visiting desk with the struggling employee, under the guise that I was evaluating overall procedures at the hospital visiting centers. It didn’t take long for me to figure out her problem.
Just after 8PM, a man walked into the lobby, right past the “Visiting Hours Are Over” sign. The visiting center staff member beamed her famous smile toward him and said cheerfully, as she always did, “Good evening. Welcome to the hospital. How can we assist you?”
“I’m here to visit a friend”, he replied. “He is a patient on the 7th floor.”
To that the woman’s huge and toothy grin seemed to even increase, and in the most pleasant and cheerful tone imaginable, she said, “Oh, I’m sorry, visiting hours ended at 8PM.”
“I just drove 45 minutes to get here,” he answered.
“I’m so sorry, Sir,” she said brightly, “but the rules say visitation after 8PM is for immediate family only.”
“Do you think this is funny?” he shot back at her. At that moment I knew exactly the nature of her problem. Her smile and cheerful nature was the only tool on her belt.
Having gone to scores of disturbance calls in hospitals over the years, I’ve observed many patterns of behavior that sparked or generated conflict and even violence. One of the things I’ve heard with great frequency from patients and visitors is, “What are you smiling at?” People have to be adaptable in their communication styles and know when to wear the appropriate expression.
Students of Vistelar’s training programs are drilled to develop a Showtime Mindset that sets the tone for communication. Proper tone and volume of voice, as well as the appropriate expression are modeled, practiced, and reinforced. That’s because it doesn’t really matter what we say, if we don’t say it well. The only way we can filter out our own moods and feelings is through practice and by raising the expectation for how staff interact with others. It’s important that everyone in professional life understands the position of advantage is ours, and the onus for setting the tone for professional relationships is on us—not on our patients, clients, and customers.
If things aren’t going well overall, then the fault partially lies in us. Ultimately, it is the fault of leaders for failing to prepare our staff through dedicated training. The stakes are high when we fail to train for what we do most as human service professionals, sales people, law enforcement officers, or anyone in a public job. And what we do most is communicate.